Toward An Understanding of Mcardle Disease: A Cross-Sectional International Questionnaire Study
Stacey L Reason1*, Renee Cadzow2, Briana J Jegier3, Amy Nwora4, Alejandro Lucia5, Andrew Wakelin6, RM Quinlivan7 and Nicol C Voermans8
1International Association for Muscle Glycogen Storage Disease, California, USA
2Department of Health, D’Youville University, Health Administration and Public Health, Buffalo, NY, USA
3Department of Health, Baptist Health Sciences University, Memphis, TN; D’Youville University, Buffalo, NY, USA
4Department of Health, D’Youville University, Health Professions Education, Buffalo, NY, USA
5Department of Sport Sciences, Universidad Europea, Madrid, Spain; PaHerg group, Research Institute Hospital, Madrid, Spain
6Association for Glycogen Storage Disease, UK
7Department of Neurology, MRC Centre for Neuromuscular Disease, Institute of Neurology, National Hospital, London, UK
8Department of Neurology, Radboud university medical center, Donders Institute for Brain, Cognition and Behaviour, Nijmegen, The Netherlands
- *Corresponding Author:
- Stacey L Reason
International Association for Muscle Glycogen Storage Disease, California,
USA,
E-mail: stacey.reason@iamgsd.org
Received date: November 29, 2022, Manuscript No. IPRDDT-22-15037; Editor assigned date: December 01, 2022, PreQC No. IPRDDT-22-15037 (PQ); Reviewed date: December 07, 2022, QC No. IPRDDT-22-15037; Revised date: December 12, 2022, Manuscript No. IPRDDT-22-15037 (R); Published date: December 15, 2022, DOI: 10.36648/2380-7245.8.12.84
Citation: Reason SL, Cadzow R, eJgier BJ, Nwora A, Lucia A, et al. (2022) Toward An Undesrtanding of Macrdle Disease: A Cross-Sectional International Questionnaire Study. J Rare Disord Diagn Ther Vol. 8 No.12:84
Abstract
Context: McArdle disease is a rare disease of skeletal muscle metabolism which is caused by a deficiency of the enzyme muscle glycogen phosphorylase. Current research literature highlights clinical features, manifestations of acute crises and varying treatment modalities; however, it fails to identify how GSDV impacts the day-to-day lives of those affected.
Objective: This patient-led tsudy aimed to enhance understanding of the day-to-day experience and healthrelated quality of life of individuals with McArdle disease (glycogen storage disease type 5).
Methods: An online survey for this patient cohort was developed, with patient reported outcomes on diagnosis, physical activity/exercise, nutrition, psychosocial aspects, pain, pregnancy, adverse events, care, and health related quality of health.
Results: Two-hundred and ninety participants across 16 countries completed the survey, which showed a long diagnostic delay, frequent misdiagnosis prior to accurate diagnosis, and co-morbidities-low-back pain, hypercholesterolemia, hypertension, (pre) diabetes and gout. A third of the participants engaged in physical activity/ exercise - mostly walking ≥ 15min, ≥5d/wk. Muscle pain/ fatigue were frequently reported as barriers to physical activity; ~1/3 of participants experienced ≥1 rhabdomyolysis episode within a 12 months period; >50% reported an emotional impact of GSDV.
Conclusions: This exploratory study examined the patient experience for individuals diagnosed with GSDV and highlights common issues.
Keywords
McArdle disease; GSDV; Patient experience; Quality of life; PROs; Patient reported outcome measures.
Introduction
McArdle disease (Glycogen Storage Disease type 5, GSDV) is a rare (prevalence of ~1/100,000 [U.S.] [1] or ~1/140,000 [Spain)] [1,2] disease of skeletal muscle metabolism which is caused by a deficiency of the enzyme Muscle Glycogen Phosphorylase (MGP). GSDV is equally represented in both sexes, and owing to the autosomal recessive pattern of inheritance, affected individuals show pathogenic mutations in both copies of the myophosphorylase-encoding gene, PYGM [2].
Individuals with GSDV typically experience physical activity intolerance and reversible acute ‘muscle crises’ (early fatigue and contractures, sometimes leading to rhabdomyolysis and subsequent myoglobinuria) triggered mostly by static muscle contractions (e.g., carrying objects) or dynamic exercise, especially when performed at vigorous intensities (e.g., moving quickly to catch a bus) [3].
An interesting and essentially universal objective phenomenon associated with GSDV, at least in adults, is the ‘second wind’ phenomenon; which is characterized by a period of less painful and more effective activity tolerance associated with a decrease in heart rate after the initial period of cramping and/or weakness [4]. This happening is an important aspect of GSDV as it does not seem to occur in other metabolic myopathies and when objectively assessed is essentially pathognomonic for GSDV [5]. ‘Second wind’ generally begins approximately ~10min after the onset of activity despite no change in work rate. Pearson et al first observed and reported this occurrence and described it as a sudden improvement in exercise tolerance associated with a decrease in pain, heart rate and dyspnea [6]. Physiologically, the ‘second wind’ represents the lag that exists in supplying sufficient energy for working muscles as a result of deficient glycolytic (i.e., ‘fast’) muscle metabolism and the time taken for the release of glucose from the liver glycogen stores-since the liver isoform of glycogen phosphorylase is not deficient in GSDV-and fatty acid oxidation (a slower metabolic pathway) to provide the required energy for working muscle fibers [4]. Some patients do not recognize the occurrence of ‘second wind’, however the occurrence thereof can be identified through objective monitoring (i.e., decrease in previous tachycardia with the use of a heart rate monitor after ~10min constant-load cycle-ergometer exercise at moderate intensities [7].
Many primary care physicians, nurses, researchers and policymakers remain largely unaware of this rare GSD, its presenting symptomatology/treatment, and the impact it has upon those affected. Current research literature highlights clinical features, manifestations of acute crises and varying treatment modalities; however, it fails to identify how GSDV impacts the day-to-day lives of those affected. Although GSDV affects a small number of individuals, it is worth noting that this cohort often becomes isolated and marginalized in healthcare systems that are more accustomed to dealing with common diseases. Limited access to specialized services, compounds the challenges around timely diagnosis and efficacious management, leaving the health of this patient cohort reliant upon conscientious self-management. The Highly Specialized McArdle Disease and Related Disorders Service in London, United Kingdom (UK) is the only known Centre of Expertise (CoE) that provides comprehensive diagnostic and ongoing disease management for a large cohort people with GSDV.
A patient-led online survey tool was developed that focused on Patient-Reported Outcomes (PROs) including: diagnosis, physical activity, nutrition, psychosocial aspects, pain, pregnancy and delivery, adverse events, access to care, and Health-Related Quality of Life (HRQoL). The aim of this cross-sectional patientled international survey was to develop a holistic understanding of the day-to-day life of individuals living with GSDV, including HRQoL in order to inform future research and the continued development of health policies, such as the use of CoEs, for this condition.
Methods
Study design and participant selection
This study used a descriptive cross-sectional design and was made internationally available to individuals and parents of children with GSDV through the online survey platform Survey Monkey. The survey was available for a period of four weeks in 2016. The inclusion criteria included: 1) having received a medical diagnosis of GSDV; 2) being able to understand English language; and 3) age ≥ 5 years. Individuals between 5–17 years were invited to involve their parents/guardians in answering the questions.
A purposive sampling approach was used, and the sampling frames included the social networking site Facebook–McArdle Disease group and the Association for Glycogen Storage Disease, UK (AGSD UK); both of which support individuals with GSDV. Institutional Review Board (IRB) approval was obtained through D’Youville University (USA). Voluntary participation in this online survey was accepted as consent.
Development of the survey tool
As there is a distinct lack of research exploring PROs in GSDV, a survey tool was developed specifically for this study, which included a validated HRQoL questionnaire, the Short Form-36 Health Survey, version 2 (SF-36v2).
A thorough literature review of the clinical impact of GSDV, along with a comprehensive audit of previous unpublished patient surveys served to inform survey development. Through extensive consultation with a patient representative for the UK CoE and the patient advocacy group: Association for Glycogen Storage Disease UK (AGSD UK), a comprehensive first draft of questions was generated. The survey tool has five sections that endeavor to capture the day-to-day experience of individuals diagnosed with GSDV: (1) Measures of Functioning and Wellbeing (Diagnosis, Physical Activity; Nutrition; Psychosocial; Pain; Pregnancy and Childbirth; Adverse Events); (2) Access and Care for GSDV; (3) Overall Health and Well-Being (SF-36v2); (4) Demographics; and (5) General comments and advice for other patients. In total there were 65 questions (Supplementary Material). The tool was piloted with six people with GSDV for readability, clarity of instructions and ease of following questions. The Flesh-Kincaid grade level for the survey was determined to be 6.4.
Statistical analysis
Descriptive statistics were predominantly used to characterize the data. Data from the SF-36v2 was analyzed with Quality Metric Health Outcomes Scoring Software 5.0. A four-week recall period was used with 2009 US general population norms. Mean t-scores were produced for the two primary measures, Physical and Mental Component Summary (MCS), and each of the eight health domains: Physical Function (PF), role limitations caused by Physical Problems, Bodily Pain (BP), and General Health (GH); MCS: Role limitations caused by Emotional Problems (RE), Vitality (VT), Social Functioning (SF), and Mental Health (MH). With norm based scoring, the average for each scale is 50 (Standard Deviation [SD]=10). The further a score falls below the norm of 50, the greater burden of illness there is. When considering group-level data, it is recommended that scores within 0.3 SD of the mean be considered within the ‘average’ or ‘normal’ range” [8]. Therefore, any health domain scale >53 or below <47 should be considered outside the normal range.
Results
Sample characteristics
In total, 290 respondents submitted completed surveys and were included in this study. Table 1 provides a summary of the demographic characteristics. The majority n=222 (77%) of respondents live in the US n=135 (47%) and UK n=87 (30%). The median age was 46 years (Inter-Quartile Range [IQR] 21). Just under half, n=139 (49%) were college graduates or higher, and n=173 (60%) were employed.
| Characteristic | n | % |
|---|---|---|
| Country (n with data=289) | ||
| Australia | 19 | 6.50% |
| Canada | 16 | 5.50% |
| Germany | 7 | 2.40% |
| Netherlands | 6 | 2.10% |
| United States of America | 135 | 46.70% |
| United Kingdom | 87 | 30.10% |
| Other* | 19 | 6.60% |
| Sex (n with data=289) | ||
| Male | 113 | 39.10% |
| Female | 176 | 60.90% |
| Age (n with data=276) | ||
| 0-14 | 4 | 1.40% |
| 15-24 | 16 | 5.80% |
| 25-40 | 84 | 31.50% |
| 41-64 | 147 | 53.30% |
| >65 | 25 | 9.10% |
| Level of education (n with data=285) | ||
| Some high school | 22 | 7.70% |
| High school graduate | 31 | 10.90% |
| Some college | 61 | 21.40% |
| Trade/tech | 32 | 11.20% |
| College graduate | 72 | 25.30% |
| Some post grad | 12 | 4.20% |
| Post graduate degree | 55 | 19.30% |
| Employment status (n with data=289) | ||
| Student | 24 | 8.30% |
| Employed Part-time | 45 | 16.60% |
| Employed Full-time | 128 | 44.30% |
| Not employed | 21 | 7.30% |
| Retired | 35 | 12.10% |
| Disabled | 60 | 19.70% |
| Attendance at CoE (n with data=284) | ||
| Yes | 60 | 21.10% |
| No | 224 | 78.90% |
| Abbreviation- CoE (Centre of Expertise). Symbol: *(Brazil, Denmark, Hong Kong, Ireland, Isle of Man, New Zealand, Portugal, Singapore, Spain, Unite Arab Emirates). | ||
Table 1: Demographic characteristics of study population.
Measures of functioning and well-being
Diagnosis: All 290 respondents indicated they had been given a medical diagnosis of GSDV. The median age at diagnosis was 29 years (IQR 20); the median age when symptoms were first experienced was 5 years (IQR 4). To fully appreciate how few people actually receive a timely diagnosis, Table 2 outlines the ages of respondents when they first experienced symptoms alongside the ages when they were diagnosed. The majority n=264 (93%) of respondents indicated that they were symptomatic prior to age 14; yet only n=32 (11%) were diagnosed before the age of symptom onset. Nearly half n=136 (48%) of the survey respondents indicated they had previously been misdiagnosed. Open-ended responses were analyzed, and the most frequently reported (medical) misdiagnosis included polymyositis, asthma, fibromyalgia psychosomatic behavior, growing pains, ‘poor fitness’ and ‘laziness’.
| Age | Diagnosis | Symptom onset |
|---|---|---|
| 0-14 | 32 (11.3%) | 264 (93.3%) |
| 15-24 | 74 (26.1%) | 9 (3.2%) |
| 25-40 | 109 (38.5%) | 7 (2.5%) |
| 41-64 | 64 (22.6%) | 3 (1.1%) |
| >65 | 4 (1.4%) | 0 (0%) |
| Total n with data = 283. Data are expressed as n (%). Note: X2(12)=27.96, p=0.006 | ||
Table 2: Age at diagnosis and symptom onset (n=283).
Overall, n=168 (59%) of respondents were diagnosed by muscle biopsy, n=47 (16%) by DNA analysis, n=54 (18%) by both, and n=20 (8%) by other means (e.g., family history, elevated Creatine Kinase (CK), non-ischemic forearm test, EMG). Baseline CK levels-a routinely assessed marker of skeletal muscle damagewere self-reported by n=172 respondents. Twenty-two percent had a baseline CK (measured in a diagnostic outpatient setting) greater than 3000 iu/L (normal range <190 iu/L); with a median value of 1400 iu/L. For males (n=56) the median baseline CK was 1450 iu/L, and for females (n=116) 1300 iu/L. The median baseline CK value across five age groups was analyzed and was found to be lower in older patients (Table 3A); although results of the nonparametric Kruskal Wallis test for the comparison of median CK values across the five age groups only showed a quasi-significant age group effect (p=0.053).
| Age | n | Mean IU/L | SD | Median IU/L | IQR |
|---|---|---|---|---|---|
| (years) | |||||
| 0-14 | 3 | 4166 | 3329 | 2500 | 3000 |
| 15-24 | 12 | 2583 | 1540 | 2250 | 1600 |
| 25-40 | 51 | 2240 | 2131 | 1200 | 1750 |
| 41-64 | 85 | 2043 | 2276 | 1200 | 1244 |
| >65 | 11 | 1298 | 1052 | 1133 | 1000 |
| Total n with data=162. Abbreviations: IQR- Inter-Quartile Range; SD- Standard Deviation. | |||||
Table 3A: Serum creatine kinase serum levels (U/L) across age groups.
Physical activity: Fifty-seven (35%) respondents reported that they engaged in physical activity lasting 15 minutes or more ≥ 5 days/week; walking (88%) was the most common activity/ exercise reported. One hundred and three (41%) respondents indicated that activity/exercise was easiest for them in the morning, compared to the afternoon (n=19 [8%]) or evening (n=14 [6%]); Thirty-eight respondents (13%) indicated they did not engage in any type of physical activity/exercise. Over half (52%) of the respondents provided a narrative response to the question ‘If you are unable or have difficulty engaging in physical activity or exercise, please identify the reason’. The two most common reasons for not exercising were ‘muscle pain’ and ‘muscle fatigue’.
Two-hundred and forty-seven (86%) respondents indicated they could achieve ‘second wind’, and of them, n=229 (85%) indicated they had improved activity/exercise tolerance once in second wind.
Table 3B shows that median baseline CK was lower in those that exercise a minimum of three days per week for at least 15 minutes. A Mann Whitney’s U test demonstrated that baseline CK was statistically lower (U=4046.5, p=0.039) for those that exercised on three or more days per week (median: 1200 iu/L, IQR 752 to 2000) compared to those that exercised on two days per week or less (2000 iu/L, IQR 1000 to 3500).
| Frequency | n | Mean IU/L | SD | Median IU/L | IQR |
|---|---|---|---|---|---|
| (days/week) | |||||
| >5 days | 57 | 1841 | 1938 | 1200 | 1300 |
| 3-4 days | 51 | 1943 | 1997 | 1200 | 1711 |
| 1-2 days | 43 | 2200 | 2115 | 1700 | 1400 |
| Not at all | 20 | 3462 | 3081 | 2500 | 4425 |
Total n with data=171. Abbreviations: IQR- Inter-Quartile Range; SD- Standard Deviation. |
|||||
Table 3B: Relationship between frequency of exercise and serum creatine kinase levels (U/L) value.
Nutrition and body mass index: One hundred and seventynine (63%) respondents indicated they do not follow any particular diet, and n=184 (68%) did not take any supplements to help manage GSDV. Body Mass Index (BMI) was calculated for all study participants that reported their weight and height (Table 4). One hundred and ninety-one (72%) participants had overweight/obesity; with the highest frequency found >41 years of age. Pearson chi-square results showed a significant direct association between BMI category and age group (X2(16)=46.28, p=0.001). A Pearson’s r post-hoc test indicated a significant but weak correlation between BMI and age (n=255, r=0.213, p=0.001).
| Age | Mean | n | SD |
|---|---|---|---|
| 0-14 | 19.8 | 4 | 2.3 |
| 15-24 | 24 | 14 | 5.07 |
| 25-40 | 28.3 | 75 | 6.94 |
| 41-64 | 29.2 | 141 | 6.23 |
| >65 | 28.7 | 24 | 5.35 |
| Total | 28.5 | 258 | 6.44 |
Average BMI across Five Age Groups (n=258) |
|||
Total n with data=258. Abbreviations: BMI- Body Mass Index; SD- Standard Deviation. |
|||
Table 4: Average Body mass index data (kg·m-2).
Emotional and psychosocial: Respondents were asked how GSDV impacts them emotionally; what their primary management concerns were; how satisfied they were with their ability to do what they wanted to; and whether they received support for emotional concerns related to having GSDV. More than half of the respondents reported an emotional impact related to living with GSDV. One hundred and sixty-five (57%) respondents often felt dissatisfied with their physical ability to do what they wanted to as a consequence of having GSDV; n=171 (59%) were often embarrassed about having to stop and rest during activity because of GSDV; and n=189 (65%) felt that others did not understand how they were feeling.
When asked what the top four concerns regarding management of GSDV were, respondents indicated the following: (1) pain; (2) exhaustion; (3) interference with daily activity; and (4) depression. To help manage emotional concerns women tended to seek out/want support more frequently than men (X2(4)=23.46, p< 0.001). Cramer’s V results showed a moderate association between gender and support for emotional concerns (V=0.292, p<0.001).
Experience of pain: All patients experienced physical activity intolerance-albeit to varying degrees and reported in various ways. Table 5 provides a summary of the themes that emerged when respondents were asked to describe the sensation(s) they felt after having pushed too hard within the first few minutes of activity.
| Thematic category | Key terms (examples) | Responses (example) |
|---|---|---|
| Pain | excruciating pain; shooting pain; muscle pain; hurts; very painful; throbbing; aching; stabbing | "Extreme pain that feels as though my muscles are being turned from muscle into stone"; "Feel pain building in muscles and pain becomes severe" |
| Cramping | charlie horse; muscle cramping; severe cramping; spasms; muscle spasms | "Sometimes I get severe cramping"; "I usually start to feel cramping in my thighs and calves" |
| Contracture | severe muscle contractures; painful contracture; instant contracture; lock up | "My muscles in the affected area contract so tightly"; "My muscles lock up, if I continue I have contractures" |
| Weakness | total weakness; weakness in general; extreme muscle weakness | "Sometimes feel weak in the thigh if walking up hill" |
| Cannot move | physically cannot move; I can't move; no energy to move; physically can't lift feet; can't move for a while; muscles seize up and can't move | "Inability to push any further onward no matter how hard I try"; "I can’t move for a little while, after a minute I can slowly starting to move my muscle"; "Muscle becomes very fatigued and heavy, to the point of not being able to move" |
| Heaviness | muscle becomes heavy; they feel heavy; calves get heavy; like walking in heavy mud; like lead weights | "Extreme heaviness if it's my legs I can't lift them"; "Like walking in heavy mud"; " Extreme heaviness if it's my legs I can't lift them, they feel like cement" |
| Tightness | acidy tightness; extreme tightness; tightening of leg muscles | "My muscles feel so tight as if I move slightly they're going to rip"; "Muscles tightening up to a point you can’t move"; "Muscles start to tighten painfully" |
| Exhaustion | distinct lack of energy; exhausted; tiredness; zero energy; drained | "A feeling as though the muscle has had its energy supply 'switched off"; "A complete depletion of energy" |
| Burning | burning pain; extreme burning; burning sensation; severe burning | "An extreme burning sensation exploding in the muscles with all thought totally over taken by the pain" |
| Shortness of breath | labored breathing; heavy breathing; breathing hard; breathlessness; out of breath | "If extreme, breath being taken away"; "Usually I'm breathing hard"; "Your breath shortens because your chest refuses to open up"; "I feel very winded" |
| Increased heart rate | extra strong heartbeat; heart rate up; heart rate is very high; heart races; pounding heart; heart rate high; intense heart beat; racing heart rate | "Heart beats faster"; "High heart rate that can make me feel sick"; "My heart will race"; "Usually I'm breathing hard and my heart will race"; "My heart rate is very high" |
| Dizziness | light-headed; faint; dizziness | " I need to sit down usually and sometimes feel dizzy" |
| Nausea | nauseous; felt sick | "Feel sick and dizzy, feel like crying sometimes" |
| Visual Disturbances | blurred vision; fuzzy vision; can't focus; bad vision | "Auras and blindness in my vision"; "Your eyesight might darken around the edges and black dots flutter " |
| Emotional | anxiety; annoyed; frustrated; angry; paranoid; despair; stress | " I feel like I have lost all of my energy and that can affect my mood"; "I have heightened anxiety as I know it will take up to 20 min until these muscles will move after I continue to rub and slowly move them"; "If with other people, I can feel anxious"; "I get completely frustrated. " |
| Total n with data = 280. | ||
Table 5: Sensation(s) felt within the first minutes of activity after having pushed too hard.
When asked how much GSDV related muscle pain interfered with various daily activities over the past four weeks, respondents indicated two activities that were moderately to extremely impacted; 63% indicated their ability to walk and move about was affected, and 70% indicated participation in recreational activities was affected.
Nearly two-thirds (n=177 [62%]) of the respondents indicated that over the past three months they experienced GSDV related muscle pain lasting for five minutes or more after activity stops, at least once/week or more.
Pregnancy and delivery: Within the total survey sample, n=123 (42.4% of total cohort; 69.9% of female participants) women indicated they had been pregnant, and of those, 44 (36%) stated they had been diagnosed with GSDV before they became pregnant. Sixty-eight (57%) women felt their exercise/ activity tolerance to be the ‘same as usual’ and n=25 (23%) women identified their tolerance to be ‘better than usual’. Of 114 deliveries, 79 (69%) were vaginal and 35 (31%) were caesarean (both planned and unplanned). Of interest, only 10% of respondents that attended the UK CoE indicated that they had a caesarean delivery, compared to 35% of those that do not attend the UK CoE.
Adverse events: The majority of respondents reported at least one episode of rhabdomyolysis (n=219 [77%]) and myoglobinuria (n=148 [53%]) over a 12-months period; recurrent episodes were frequent (26.8% experienced more than six episodes). Lifetime occurrence of renal failure (3%) and compartment syndrome (13%) was low/infrequent (Table 6).
| Rhabdomyolysis * (n=284) | Myoglobinuria** (n=281) | Renal failure (n=280) | Compartment syndrome (n=281) | |
|---|---|---|---|---|
| past 12 months | past 12 months | past 12 months | lifetime occurrence | |
| No | 65 (22.9%) | 133 (47.3) | 272 (97.1%) | 246 (87.5%) |
| Yes | 35 (12.5%) | |||
| 1-2 times | 91 (32.0%) | 98 (34.9%) | 4 (1.4%) | |
| 3-5 times | 52 (18.3%) | 31 (11%) | 4 (1.40%) | |
| > 6 times | 76 (26.8%) | 19 (6.8%) | 0 (0%) | |
| Data are expressed as n (%). Note: *X2(3) = 10.36, p = 0.01; **X2(3) = 11.12, p | ||||
Table 6: Patient-reported outcomes regarding adverse events.
Access and care for GSDV
Eighty-seven (30%) respondents identified they live in the UK, and of those, 60 (21%) indicated they attended the UK CoE. In Canada, 4 of 15 respondents (27%) were seen by a GSDV specialist (defined in the survey as a medical doctor that has specialized education and training related to GSDV, and actively provides care to GSDV patients); in the US, 9 of 153 respondents (7%) did. Patients reported benefit from care by GSDV specialists.
Of the patients that reported they did not attend a CoE, 56% had never seen a specialist. Nearly half (49%) of these respondents visited their general practitioner at least once a year to manage their condition, compared to 25% of respondents that attended the UK CoE for the same time period. The two primary reasons cited for not seeing a GSDV specialist amongst those who did not attend a CoE were: ‘I cannot find a GSDV specialist’ (20%) and ‘there is not a GSDV specialist in my area’ (49%). Ten percent of respondents expressed: (1) there is no benefit; (2) pointless; (3) doctor doesn’t know much; (4) they were given wrong information; or (5) not helpful.
For those admitted to hospital with rhabdomyolysis (n=140), ‘extreme muscle pain’ (n=112 [79%]) was the most frequently reported symptom that prompted admission; followed by ‘high CK’ (n=37 [68%]), ‘dark urine’ (n=95 [67%]), and ‘feeling very unwell’ (n=92 [65%]). Additional, narrative responses regarding symptoms that prompted admission included renal failure, vomiting, and compartment syndrome. As expected, ‘anaerobic activities’ (n=88 [62%]) was the predominant cause that precipitated symptoms. While others, such as ‘activity when stressed or tired’ (n=31 [22%]) and ‘holding an awkward position’ (n=28 [20%]) were cited less often. The median length of stay in hospital for these respondents was 5 days (IQR 4).
Nearly three quarters (n=210 [73%]) of respondents indicated they have received support from a community-based organization. Open-ended questions were analyzed, and three main responses emerged: (1) GSDV Facebook group (n=124 [59%]); (2) AGSD UK (n=55 [26%]); and (3) Muscular Dystrophy Association (MDA) (n=22 [11%]). Of note, the International association for muscle Glycogen Disorders (IamGSD) was established in 2017.
Overall health and well-being
General Health: Respondents were asked to identify whether they had other existing health conditions. Sixty (23%) respondents indicated they did not have any other health conditions. Seventy seven percent indicated they did; including lower back pain (n=120 [46%]), hypercholesterolemia (n=79 [31%]), hypertension (n=70 [27%]), (pre) diabetes (n=42 [16%]), gout (n=24 [9%]), coronary artery disease (n=16 [6%]), and various other comorbidities (n=85 [33%]).
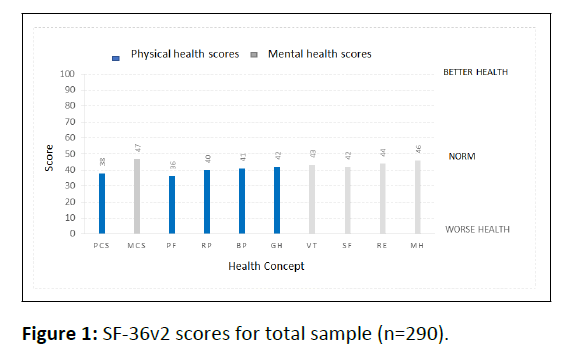
Health Related Quality of Life: Figure 1 presents mean tscores for the total sample of individuals with GSDV (N=290). The PCS and MCS scores summarize the group’s physical and mental health status. The PCS score (38) for this sample is well below the normal range, indicating substantial limitations in selfcare, physical, social and role activities; severe bodily pain; frequent tiredness; and health rated as poor [8] Only 3% were above the norm, 20% at the norm, and 77% below the norm. The MCS score for this sample was 47, and therefore considered within the normal population range. Nearly a third of the sample (30%) was above the general population norm, third (31%) at the norm, and 39% below the norm.
Abbreviations: PCS-Physical Component Summary: MCS-Mental Component Summary: PF-Physical Function: RP-Physical Role Functioning: BP-Bodily Pain: GH-General Health: VT-Vitality: SF-Social role Functioning: RE-Emotional Role Functioning: MH-Mental Health.
Because the score of the PCS measure was in the impaired range, further examination of the four related health domains was warranted; with PF being the most representative physical health measure. The PF score for this group was the lowest of all measures (i.e., 36). Items associated with the PF measure (vigorous/moderate activities, lifting or carrying groceries, climbing several flights of stairs, climbing one flight of stairs, bending and kneeling, walking a mile, walking several blocks, walking one block, and bathing/dressing) are typical activities that individuals with GSDV generally have difficulty with, so this finding is not surprising.
General comments including advice for patients
Recognizing the patient as ‘expert’ uncovers valuable insights and grass-roots counsel. Respondents were asked what advice they would provide to someone that was newly diagnosed with GSDV. Table 7 presents a summary of the emergent themes surrounding patient advice, including advice on informing themselves and their surroundings, finding a medical expert and keeping physically fit.
| Thematic category | Key terms (examples) | Responses (examples) |
|---|---|---|
| Educate yourself about McArdle disease | do research; get educated; read | "Learn about your condition"; "Find out as much as possible"; "Use the internet to get information" |
| Find a doctor that knows about McArdle disease | find a good doctor; physician with McArdle experience; seek expert help | "Find a McArdle's specialist"; "Try and go to the London clinic"; "Find a doctor that knows about the problem" |
| Get support from family, friends, support groups | join AGSD UK; join Face Book group; counselor | "Find support through doctors, counselors, or Face Book"; "Find a support group"; "Stay in touch with others that have the disease" |
| Advise others about your limitations | explain to others; tell people | "Make sure people know you have the disease"; "Educate family and friends"; "Do not keep it a secret"; "Explain to friends so you can stop and rest when necessary" |
| Don't be embarrassed | don't be embarrassed; try not to be embarrassed | "Try not to be embarrassed, it makes things worse"; "Don't be ashamed or embarrassed when you need to rest" |
| Listen to your body and know your limits | listen to your body; know your limits; live within them; pace yourself' don't force beyond limits | "Know your limits, don't force yourself past them"; "Listen to your muscles, if it hurts slow down"; "Even though your mind tells you to keep going, listen to your body" |
| Don't push through the pain - stop or slow down and rest | do not push yourself; don't overdo it; take it slow and steady | "Stop and rest when you start to feel any pain"; "You can still push yourself, you just have to figure out your limits"; " Adapt activities to avoid muscle pain" |
| Learn about second wind | 2nd wind; importance of second wind; supervised second wind | "Understand second wind"; "exercise in second wind every day"; "The second wind phenomenon is a major key" |
| Stay active | exercise daily; keep active; workout everyday | "Daily walks"; "Encourage you to exercise daily"; "If you don't keep moving things get worse"; "As hard as it is, keep active" |
| Maintain a healthy weight | avoid weight gain; watch your weight | "Do not get overweight"; "Maintain your ideal weight"; "Lose weight if you're overweight" |
| Have a good attitude | live your life; don't give up; accept your condition | "You can live a full life" "Don't sweat the small stuff"; "Be kind to yourself"; "Take it easy"; "Get on with life"; "You can live a full and amazing life" |
| You are not alone | you’re not alone; talk to others | "It's not just you, there is good help out there"; "You're not alone in this, and you're not crazy" |
n with data = 260 |
||
Table 7: Patient advice for newly diagnosed patients.
Discussion
Insight into the patient experience is important for researchers, clinicians, and policy-makers, as it provides another dimension of understanding beyond clinical presentation. This study addressed the current gap in knowledge on PROs and HRQoL for individuals diagnosed with GSDV and expounds common issues this cohort faces concerning diagnosis, physical activity, nutrition, psychosocial, pain, pregnancy and childbirth, adverse events, general health, and access/care.
While 16 countries were represented in this study, a disproportionate number of participants (77%) lived in the UK (n=87 [31%]) and US (n=135 [47%]). This is likely to be related to the sampling frames used (Facebook and AGSD UK), the population density of these countries, country-specific rates of diagnosis, and language barriers in non-English speaking countries. The median age for this sample was 46 years, and the median age at diagnosis 29 years, both very similar to the recently reported European cohorts [6-8]. The rate of disability was slightly higher for this group than the approximate global rate of 15% [9].
The survey showed a long diagnostic delay and frequent misdiagnosis prior to a definitive diagnosis, including polymyositis, asthma, and fibromyalgia; while less formal misdiagnosis consisted of psychosomatic behavior, growing pains, laziness, and poor fitness. This is similar to previous findings in the UK; this population has a partial overlap with the current study [10]. These findings are noteworthy in consideration of how important early diagnosis and adoption of an appropriate lifestyle is in helping to improve HRQoL and in preventing severe life-threatening complications [11]. Increased awareness of GDSV amongst primary care physicians, coupled with recognition of typical symptoms associated with physical activity intolerance are necessary for timely diagnosis.
Our survey demonstrated that not all patients received gold standard diagnostic testing, namely genetic confirmation with or without muscle biopsy. Some respondents were diagnosed by muscle biopsy alone, and more alarmingly some were diagnosed by forearm exercise testing alone.
Baseline CK is usually higher than 1000 iu/L for individuals with GSDV [7]. Comparatively, our sample (n=162) had a median baseline CK of 1400 IU/L. As this research did not objectively confirm a positive diagnosis of GSDV amongst participants, a median self-reported baseline CK >1000 iu/L further supports a positive diagnosis for these participants.
Prior to second wind, many individuals struggle with physical activity intolerance in daily activities. Although most respondents indicated they were able to achieve ‘second wind’, many indicated that pain interfered with physical activity. While only a minority indicated they did not engage in physical activity or exercise; over half stated that ‘muscle pain’ and ‘muscle fatigue’ were the predominant reasons for reduced physical activity. These descriptors are commonly associated with impaired muscle glycolysis and represent a roadblock for continued activity. Without proper guidance, managing activity during this adaptation phase can be difficult. At the very least, ineffective management results in repeated episodes of muscle pain and fatigue; and possibly serious adverse events such as rhabdomyolysis with potential risk of acute renal damage.
As such, one of the goals for effective day-to-day management is for individuals to recognize the emblematic symptoms (early fatigue, weakness of muscles being used, and pain), and slow down or stop until alternate energy substrates for skeletal muscle become available (‘second wind’ phase). This will reduce the sensation and duration of pain. Continued activity despite the initial sensation of pain can trigger muscle spasms or contractures and will often lead to muscle damage. Respondents described the sensations they feel during the first minutes of activity after having pushed too hard. For primary care physicians, awareness of these common sensations, particularly when accompanied by the experience of ‘second wind’, can serve as an important screening tool when assessing undiagnosed patients.
Two-thirds of respondents indicated they engaged in physical activity lasting 15 minutes or more on three or more days a week. While it is encouraging that two-thirds of the respondents engage in regular exercise, it is less than the current optimal exercise recommendation of 30 minutes on at least five days per week [2]. In healthy individuals, aerobic exercise is known to improve the ability of muscles to burn fat for energy during exercise. For individuals with GSDV, regular activity leads to improved aerobic capacity, which in turn helps to improve physical activity tolerance [12]. Patients fulfilling leisure time international physical activity recommendations (i.e., 150 or more minutes per week in moderate-vigorous aerobic activities) indeed showed higher cardiorespiratory fitness and physical HRQoL scores than those not meeting guideline recommendations [13]. Furthermore, we found that median baseline CK was lower with more frequent physical activity, in line with previous findings [3,13,14].
The lack of consensus regarding nutritional and pharmacologic management is clearly reflected in this study sample. Two-thirds of participants in this study do not follow a particular diet or take any supplements (e.g., sports drinks before exertion) to help manage GSDV. An informal survey (n=38) exploring the use of a ketogenic diet for GSDV management showed improvement in everyday symptoms and exercise tolerance in the majority of patients [11,15]. Results from a recent (2022) randomized placebo-controlled, crossover study that investigated the effects of a modified ketogenic diet in patients with GSDV is expected to inform dietary recommendations for this patient group [11,15,16]. Furthermore, nearly half of the respondents stated exercise was easier for them in the morning. A follow-up question on the survey tool to clarify whether this was related to an overnight fast or not would have been informative.
In 2016, the World Health Organization (WHO) stated that 39% of adults aged >18 years had overweight and 13% had obesity [17]. Of respondents >18 years, nearly three-quarters had overweight and obesity (38% and 34% respectively). This PRO is of great concern; not only is obesity linked to various chronic health conditions, but it very likely contributes to the ongoing challenges patients with GSDV face regarding physical activity intolerance and achieving aerobic fitness, which in turn negatively affects the ability to maintain a healthy weight [12, 13].
For many, the impact of living with a rare disease is profound, often contributing to various emotional concerns. Lack of diagnosis, misdiagnosis, and/or a delay in diagnosis further accentuates the emotional burden [10]. For years, individuals struggle to understand and manage their activity intolerance; never being able to keep up or fit in amongst their peers. While the physiologic effects are generally understood; the psychological imprint has not been widely studied.
In light of identified emotional sequelae, the need for a multifaceted approach to patient care is underscored. Access to professional psychological care is warranted to effectively manage these feelings. At the UK CoE, a neuropsychologist is an integral member of the multidisciplinary team. Attending to the psychological needs of patients ensures appropriate screening for issues such as anxiety, depression and feelings of dissatisfaction. Psychological support can also be helpful to increase motivation to exercise regularly. For those in need of treatment, cognitive behavioral therapy is available, along with referral to and liaison with local psychology services for on-going treatment.
This study found women were more likely to seek out/want support to address emotional concerns, drawing attention to yet another common barrier that exists between gender and psychological care [11]. The findings from this survey call for continuous attention for psychological coaching and physical activity training for both newly diagnosed patients and those needing further support. To identify facilitators and barriers to coping with the limitations of GSDV, we will perform a subsequent international survey focusing on how patients learn to live with GSDV.
The interplay between GSDV and pregnancy has not been fully investigated. Anecdotal reports suggest some expectant mothers experience improved physical activity tolerance; however, this study found only a quarter of respondents reported their physical activity tolerance was better than usual. Nash et al., (2022) present two GSDV case reports where CK levels were stable or slightly lower than baseline CK throughout the antepartum period [18]. The WHO reports a global caesarean rate of 1 in 5 (21%) of all childbirths [19]. A literature review that included 15 papers and 35 cases, reported a 37% incidence of cesarean birth amongst women with GSDV compared to our finding of 31% [18]. The question that must be addressed is whether a cesarean rate >30% for women with GSDV is medically necessary. Of interest, only 10% of women attending the UK CoE report having a cesarean birth. Nash (2022) states that women can successfully deliver vaginally, with consideration of an assisted second stage recommended to reduce the risk of postpartum rhabdomyolysis [18]. Further research is needed to better understand how GSDV affects pregnancy/labor. Most likely, a careful exercise adaptation training program may be advisable to minimize labor risks [11].
The relationship between various chronic health conditions and GSDV is not well understood. Point prevalence was established for a variety of chronic health conditions. Two measures in particular stood out as being more prevalent amongst our sample compared to the general population. The prevalence of gout for this sample was 9%, which is more than twice the global rate of 1-4% [20]. In the recent UK observational study, the incidence of gout and hyperuricaemia were even higher [21]. This is likely due to impaired ATP production with resultant hyperuricemia [3, 21]. Low back pain was reported to be 46% for this sample, higher than the global point prevalence of 12% (SD=2.0) [22]. This might be related to paraspinal muscle wasting and weakness in GSDV [23]. Country specific analysis, alongside retrospective chart reviews would provide a more comprehensive picture of the prevalence and trends of chronic health disease amongst patients with GSDV.
Although GSDV is not typically considered a life-threatening condition, adverse events such as rhabdomyolysis and renal failure can potentially be life threatening, and for those who incur an adverse event, aerobic capacity is often impacted during the recovery phase; thereby further reducing functional ability. An important message for all patients requiring hospitalization, regardless of the reason, is to understand what factors contributed to their admittance, and to learn strategies to avoid future episodes. Over and above educating patients about how to avoid these events (through effective day-to-day management), there is a need to provide emergency guidelines to individuals regarding prompt assessment and medical management, and to impart strategies for regaining aerobic fitness [11].
To address geographic health inequalities and gaps in knowledge, individuals often turn to the internet. The McArdle Disease Facebook group was the most frequently reported source for information and support, with the AGSD UK second. As more patients sought information online, the need for an international PAO became evident. As such, IamGSD was established (2017). This PAO supports individuals with muscle GSDs and strives to raise awareness, provide support, advocate the patient viewpoint, disseminate best practice, and contribute to research.
Continued efforts must be made to raise awareness of GSDV amongst healthcare providers, in particular primary care physicians and ED doctors. By doing so, affected individuals will be more likely to receive an early and correct diagnosis, which in turn will improve PROs for this patient group. To achieve this, potential areas for policy development should include: enhancing content on GSDs in family and emergency medicine residency programs, offering continuing medical education credits that focus on identification and treatment of GSDs, and through an increased use of next generation sequencing [24,25].
The formation of IamGSD, and a Europoean Union grant to fund EUROMAC (an international network and registry which included specific training for some low income countries) have been very important steps [26]. Establishment of published of Clinical Practice Guidelines (CPGs) for GSDV management is another important development [11]. Assessing and evaluating the HRQoL of patients with GSDV is an important component in the provision of comprehensive patient care. HRQoL represents a practical and cost-effective measure in clinical practice, which ultimately enables healthcare providers to better meet the needs of patients and families [26,27].
Overall, mean SF-36 scores for this population were lower in the physical domains than they were for the mental domains. Given the inherent features of this metabolic myopathy, a low PCS score is not surprising. The hallmark symptom of activity/ exercise intolerance is reflected in a low PF score, and as previously discussed, muscle related pain is often synonymous with premature exertional fatigue, resulting in a low BP score for this group as well. The combination of activity/exercise intolerance and muscle pain likely contributes to a low RP score.
Although the MCS score is within normal limits, the four related health domains (VT, SF, RE, and MH) were all below the normal range. These scores are congruent with previously reported findings regarding an increased sense of frustration, feelings of embarrassment, and lack of understanding from others. Respondents also indicated concerns regarding the interference of GSDV with their daily activities and concerns surrounding depression.
While clinical, objective data is of the utmost importance, the subjective experience adds a layer of understanding and authenticity that only those who have experienced the phenomenon at hand can provide. The advice respondents dispensed was in large part in accordance with main-stream recommendations; however, the more elusive lessons are worth observing-educate yourself; get support from family, friends, support groups; advise others about your limitations; don’t be embarrassed; have a good attitude; and you are not alone. Not only do these recommendations capture the first-hand experience of those affected, they illuminate the benefits of hindsight [27].
Limitations and Strengths
This study is not without limitations. Design of a representative sample for surveying a rare population can be challenging, as such a convenience sample was used. The primary concern associated with this method is that the sample is not representative of the entire population. As this is the largest known patient-driven study on GSDV, and the only one exploring the day-to-day experience, we do not have any data to compare the demographic characteristics of our convenience sample to recent other cohorts reported [2,28]. Data was selfreported through an online survey, therefore, inherent limitations associated with social desirability and recall bias may exist. An assumption was made that participants responded honestly about their overall health and experience with GSDV. The survey was only available in English, and therefore did not capture PROs from non-English speaking respondents. Lastly, this study did not account for the fundamental differences in healthcare delivery systems between countries and the impact these variances may have on PROs.
Next, the data was obtained in 2016 and reported in 2022. This publication delay is related to the priority given to the development of recommendations for patients online by the foundation of the international PAO IamGSD, and for physicians by the composition of CPGs [11]. The data obtained in this survey paved the way for these two important initiatives. Following the publication of these CPGs we have continued with this report.
Conclusion
To our knowledge, this is the largest patient-led survey of individuals with GSDV exploring both the individual day-to-day experience, and HRQoL. This study presents an in-depth description of the unique experience of individuals affected by GSDV. While the primary focus of this study was descriptive in nature, this data also serves to inform further research in order to better understand how GSDV affects pregnancy, the potential risk/benefit of a ketogenic diet, and whether certain chronic diseases are more prevalent amongst this cohort and the implications thereof. Furthermore, by eliciting a deeper understanding of the patient experience, clinicians will be better equiped to meet the unique needs of this cohort.
Lastly, to effect change, national and regional policies are needed to alter the present course toward a path that is illuminated with enhanced access and dissemination of patientinformed universal guidelines; with the ultimate goal of improving HRQoL for all individuals with GSDV.
Acknowledgements
We are grateful to all respondents of the survey and to IAMGSD for supporting the conduction of the survey. The authors would like to acknowledge Dr. Jatin Pattni for providing expert opinion on content development for the survey tool.
References
- Castro De, Johnston MJ, Biesecker L (2015) Determining the prevalence of McArdle disease from gene frequency by analysis of next-generation sequencing data. Genet Med 17: 1002-1006.
[Crossref], [Google Scholar], [Indexed]
- Santalla A, Nogales-Gadea G, Glazquez Encinar A, Vietez A, Gonzalex-Quintana A, et al. (2017) Genotypic and phenotypic features of all Spanish patients with McArdle disease: a 2016 update. BMC Genomics 18: p819.
[Crossref], [Google Scholar], [Indexed]
- Lucia A, Nogales-Gadea G, Perez M, Martin MA, Andreu AL, et al. (2008) McArdle disease: what do neurologists need to know?. Nat Clin Pract Neurol 4: 568-577.
[Crossref], [Google Scholar], [Indexed]
- Scalco RS, Chatfield S, Godfrey R, Pattni J, Ellerton C, et al. (2014) From exercise intolerance to functional improvement: The second wind phenomenon in the identification of McArdle disease. Arq Neuropsiquiatr 72: 538-541.
[Crossref], [Google Scholar], [Indexed]
- Miteff F, Potter HC, Allen J, Teoh H, Roxburgh R, et al. (2011) Clinical and laboratory features of patients with myophosphorylase deficiency (McArdle disease). J Clin Neurosci 18: 1055-1058.
[Crossref], [Google Scholar], [Indexed]
- Pearson CM, Rimer DG, Mommaerts WF (1961) A metabolic myopathy due to absence of muscle phosphorylase. Am J Med 30: 502-517.
[Crossref], [Google Scholar], [Indexed]
- Salazar-Martinez E, Santalla A, Valenzuela PL, Nogales-Gadea G, Pinos T, et al. (2021) The Second Wind in McArdle Patients: Fitness Matters. Front Physiol 12: p744632.
[Crossref], [Google Scholar], [Indexed]
- Maruish ME, Kosinski M, Bjorner J, Maruish ME, Kosinski M, et al. (2011) User’s Manual for the SF-36v2 Health Survey. 3rd Edition, Quality Metric Incorporated.
- G.B.D 2017 Disease and Injury Incidence and Prevalence Collaborators (2018) Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 392: 1789-1858.
[Crossref], [Google Scholar]
- Scalco RS, Morrow JM, Booth S, Chatfield S, Godfrey R, et al. (2017) Misdiagnosis is an important factor for diagnostic delay in McArdle disease. Neuromuscul Disord 27: 852-855.
[Crossref], [Google Scholar], [Indexed]
- Lucia A, Martinuzzi A, Nogales-Gadea N, Quinlivian R, Reason SL (2021) Clinical practice guidelines for glycogen storage disease V & VII (McArdle disease and Tarui disease) from an international study group. Neuromuscul Disord 31: 1296-1310.
[Crossref], [Google Scholar], [Indexed]
- Quinlivan R, Vissing J, Hilton-James D, Buckely J (2011) Physical training for McArdle disease. Cochrane Database Syst Rev 12: Cd007931.
[Crossref], [Google Scholar], [Indexed]
- Munguia-Izquierdo D, Santalla A, Lucia A (2015) Cardiorespiratory fitness, physical activity, and quality of life in patients with McArdle disease. Med Sci Sports Exerc 47: 799-808.
[Crossref], [Google Scholar], [Indexed]
- Lucia A, Ruiz JR, Santalla A, Nogales-Gadea G, Rubio JC, et al. (2012) Genotypic and phenotypic features of McArdle disease: Insights from the Spanish national registry. J Neurol Neurosurg Psychiatry 83: 322–328.
[Crossref], [Google Scholar], [Indexed]
- Reason SL, Lokken N, Voermans N (2021) International patient group harnesses social media to help inform rare disease research: Use of a low carbohydrate ketogenic diet in McArdle disease. Curr Opin Endocrinol Diabetes Obes 28: 441-445.
[Crossref], [Google Scholar], [Indexed]
- Lokken N, Hansen KK, Storgaard JH, Orngreen MC, Quinlivan R et al. (2020) Titrating a modified ketogenic diet for patients with McArdle disease: A pilot study. J Inherit Metab Dis 43: 778-786.
[Crossref], [Google Scholar], [Indexed]
- Chooi YC, Ding C, Magkos F (2019) The epidemiology of obesity. Metabolism 92: 6-10.
[Crossref], [Google Scholar], [Indexed]
- Nash CM, Shetty N, Miller A, McCoy K (2022) McArdle disease and pregnancy: A case report and scoping review of pregnancy outcomes. Obstet Med 15: 40-44.
[Crossref], [Google Scholar], [Indexed]
- World Health Organization (2022) Caesarean section rates continue to rise, amid growing inequalities in access.
- Dehlin M, Jacobsson L, Roddy E (2020) Global epidemiology of gout: Prevalence, Incidence, treatment patterns and risk factors. Nat Rev Rheumatol 16: 380-390.
[Crossref], [Google Scholar], [Indexed]
- Pizzamiglio C, Mahroo OA, Khan KN, Patasin M, Quinlivan R (2021) Phenotype and genotype of 197 British patients with McArdle disease: An observational single-centre study. J Inherit Metab Dis 44: 1409-1418.
[Crossref], [Google Scholar], [Indexed]
- Hoy D, Bain C, Williams G, March L, Brooks P, et al. (2012) A systematic review of the global prevalence of low back pain. Arthritis Rheum 64: 2028-2037.
[Crossref], [Google Scholar], [Indexed]
- Alvarez-Velasco R, Nunez-Peralta CA, Alonso-Perez J, Gallardo E, Collet-Vidiella R, et al. (2022) High prevalence of paraspinal muscle involvement in adults with McArdle disease. Muscle Nerve .
[Crossref], [Google Scholar], [Indexed]
- Scalco RS, Snoeck M, Quinlivan R, Treves S, Laforet P, et al. (2016) Exertional rhabdomyolysis: physiologicalresponse or manifestation of an underlying myopathy?. BMJ Open Sport & Exer Med 2: e000151.
[Crossref], [Google Scholar], [Indexed]
- Fernandes PM, Davenport RJ (2019) How to do it: investigate exertional rhabdomyolysis (or not). Practical Neurology 19: 43-48.
[Crossref], [Google Scholar], [Indexed]
- Pinos T, Andreu AL, Bruno C, Hadjigeorgiou GM, Haller RG, et al. (2020) Creation and implementation of a European registry for patients with McArdle disease and other muscle glycogenoses (EUROMAC registry). Orphanet J Rare Dis 15: 187.
[Crossref], [Google Scholar], [Indexed]
- Quinlivan R, Andreu AL, Martin R (2017) 211th ENMC International Workshop:: Development of diagnostic criteria and management strategies for McArdle Disease and related rare glycogenolytic disorders to improve standards of care. 17-19 April 2015, Naarden, The Netherlands. Neuromuscul Disord 27: 1143-1151.
[Crossref], [Google Scholar], [Indexed]
- Scalco RS, Lucia A, Santalla A, Martinuzzi A, Vavla M, et al. (2020) Data from the European registry for patients with McArdle disease and other muscle glycogenoses (EUROMAC). Orphanet J Rare Dis 15: p330.
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences