Thoughts on the Application of High Flow Nasal Cannula Oxygen Therapy in Patients with Severe Pneumonia: A Case Report and Review of Literature
Dezhu Tang, Xiaohui Zhou, KeXiong Lin, and Yun Wan
DOI10.36648/2380-7245.21.7.25
Dezhu Tang†, Xiaohui Zhou†, KeXiong Lin and Yun Wan*
Department of Respiratory and Critical Care Medicine, The Second Hospital of Jiulongpo District, Chongqing, Chongqing-400052, P.R. China
†Dezhu Tang, Xiaohui Zhou Co-First Authors
- *Corresponding Author:
- Yun Wan
Department of Respiratory and Critical Care Medicine
The Second Hospital of Jiulongpo District
Chongqing, Chongqing-400052, P.R. China
E-mail: 3150499292@qq.com
Received Date: June 16, 2021; Accepted Date: July 12, 2021; Published Date: July 23, 2021
Citation: Tang D, Zhou X, Lin K, Wan Y (2021) Thoughts on the Application of High Flow Nasal Cannula Oxygen Therapy in Patients with Severe Pneumonia: A Case Report and Review of Literature. J Rare Disord Diagn Ther Vol.7 No.7:25.
Abstract
For severe pneumonia that requires respiratory support, non-invasive mechanical ventilation (NIV) is usually the first choice, but in recent years, high-flow nasal cannula (HFNC) oxygen therapy has also appeared in critically ill patients. We reported an 85-year-old male presented to our hospital that suffered from hypoxic respiratory failure due to dry cough and fever for a day and was diagnosed with severe pneumonia. HFNC therapy was first given to him, but the patient's condition progressed and oxygen saturation decreased, so we used NIV as respiratory support. However, the patient could not tolerate the NIV, so we changed it to HFNC again and adjusted the parameters. The patient's discomfort was improved, and he was finally discharged from the hospital after his condition improved. In conclusion, HFNC may be an alternative means of respiratory support for patients with severe pneumonia.
Keywords
Severe pneumonia; High-flow nasal cannula; Non-invasive mechanical ventilation
Introduction
Community-acquired pneumonia (CAP) is an important public health problem and a major cause of morbidity and mortality worldwide [1,2]. Pneumonia in the elderly happens fast and the prognosis is poor, and elderly are susceptible to severe pneumonia with mortality rate as high as 20% [3,4]. In intensive care unit (ICU), half of CAP required mechanical ventilation [5]. We report a patient who had hypoxic respiratory failure was changed to high-flow nasal cannula (HFNC) due to poor tolerance to non-invasive mechanical ventilation (NIV).
Case Presentation
An 85-year-old male presented with dry cough and fever (body temperature unmeasured) for one day accompanied by nausea, vomiting, and chest pain, as well as dyspnea, no hemoptysis, chest tightness, profuse sweating, syncope, etc. Upon examination, the pulse was 114 beats/min, the blood pressure was 130/80mmHg, the respiratory rate was 31 breaths/min, and the body temperature was 37.4℃. Physical examination showed normal consciousness, low breathing in lungs, no rhonchus or moist rale. Heart and abdominal examination showed no obvious positive signs.
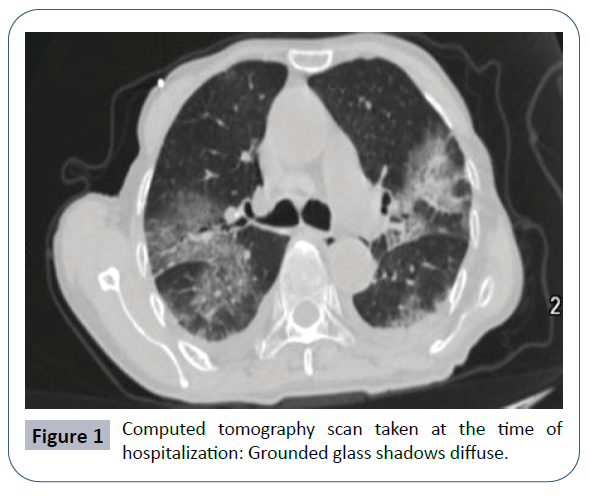
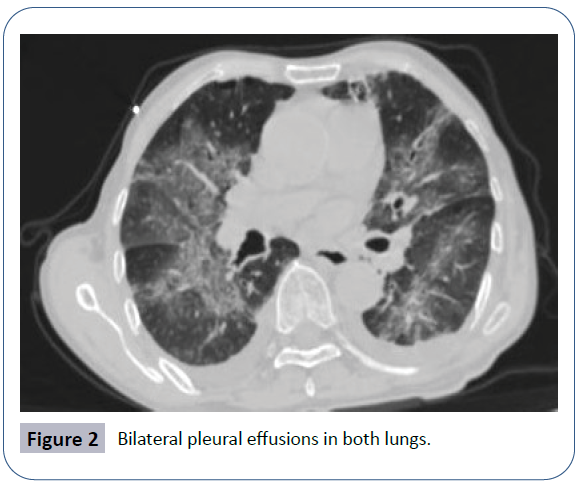
Laboratory studies showed that white blood cell count was 1.86 × 10-9/L (normal reference range 4 × 10-9/L-10 × 10-9/L), neutrophil percentage was 80.70% (normal reference range 50% to 70%, hemoglobin was 137.00 g/L, platelet count was 37.00 × 10-9/L), procalcitonin was 16.48 ng/mL, D - Dimer was 1.04 ug/mL, renal function and troponin was normal. The influenza virus, COVID-19 nucleic acid test and mycoplasma test were all negative. Arterial blood gas (nasal catheter oxygen therapy 3 L/min) showed that PH was 7.411 mmHg, PO2 was 47.9 mmHg, PCO2 was 34.2 mmHg D1 (Table 1). Chest computed tomography showed that scattered ground glass density shadows and bilateral pleural effusion in both lungs (Figures 1 and 2).
| Length of stay | Respiratory support | FIO2 (%) | PH | PO2 (mmHg) | PCO2 (mmHg) | HCO3- (mmol/L) | BE (mmol/L) | SO2 (%) |
|---|---|---|---|---|---|---|---|---|
| D1 | Nasal catheter oxygen therapy | 33 | 7.427 | 83 | 35.5 | 23 | -0.4 | 96.7 |
| D2 | Nasal catheter oxygen therapy/HFNC* | 33 | 7.385 | 44.8 | 36.9 | 21.6 | -2.5 | 77.1 |
| D3 | HFNC | 45 | 7.457 | 58.7 | 30.6 | 21.3 | -1.5 | 91.3 |
| D4 | NIV/HFNC† | 53 | 7.457 | 46.8 | 29.2 | 20.3 | -2.2 | 82 |
| D5 | HFNC | 70 | 7.444 | 53.2 | 31.5 | 21.2 | -1.6 | 85.3 |
| D6 | 70 | 7.424 | 68.5 | 34 | 21.8 | -1.5 | 92.8 | |
| D7 | 66 | 7.488 | 150 | 34.2 | 25.7 | 2.5 | 99.4 | |
| D8 | 45 | 7.454 | 86.5 | 38 | 26.9 | 2.3 | 96.4 | |
| D9 | 40 | 7.479 | 96.5 | 40.7 | 29.9 | 6.2 | 98.1 | |
| D10 | nasal catheter oxygen therapy | 27 | 7.466 | 98.6 | 43.6 | 31 | 6.8 | 97.9 |
| D11 | 27 | 7.452 | 95.9 | 37.9 | 26.1 | 2.4 | 98.1 |
Table 1: The result of arterial blood gas.
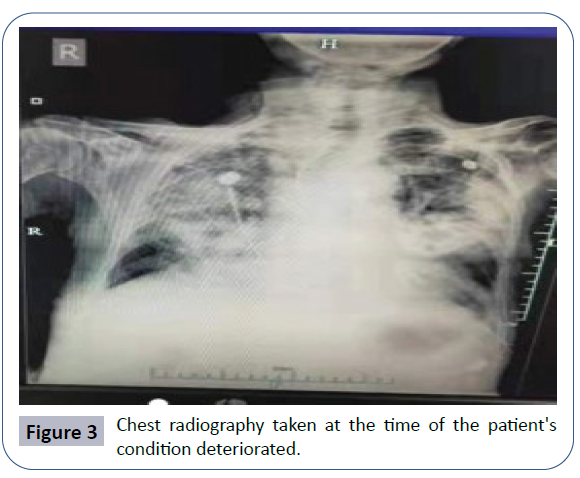
Our team diagnosed the patient with severe pneumonia and formulated anti-infective treatments for patients with piperacillintazobactam, moxifloxacin and oseltamivir (Table 2). Re-checking blood gas analysis on the second day of hospitalization indicated that the oxygenation index was lower than that of the day of admission D2 (Table 1). In view of the patient's no unconscious disorder, no dysphagia, no difficulty in expectorating sputum and other risks, we first used HFNC oxygen therapy and set the fraction of inhaled oxygen (FIO2 %) at 45%, the flow rate at 20L/min, and the temperature at 33°C, and his peripheral finger oxygen saturation maintained at 89%-93%. But on the third night of hospitalization the patient’s dyspnea worsened, re-checking the arterial blood gas (Table 1) D3 indicated that the oxygenation index decreased, and the chest radiographs (Figure 3) indicated that lung lesions increased. Six hours later, the patient's peripheral finger oxygen saturation decreased to 81%. After discussion, we changed to NIV as respiratory support. About 30 minutes later, the patient’s peripheral finger oxygen saturation increased to 88% while the patient felt obviously dyspnea and couldn’t tolerate it.
| Moxifloxacin (0.4 g/qd) | Piperacillin-Tazobactam (4.5 g/q8h) | Oseltamivir (75 mg/bid) | Methylprednisolone sodium succinate (40 mg/qd) |
|---|---|---|---|
| D1~D17 | D1~D11 | D3~D10 | D4~D7 |
Table 2: The main drugs used during hospitalization.
The patient refused to continue using NIV and was emotionally irritable, re-checking blood gas analysis indicated that the oxidation index was further deteriorated (Table 1) D4, so we used HFNC oxygen therapy again, and adjusted the FIO2 % to 70% and the flow rate to 45 L/min. The patient felt that the symptoms of dyspnea had improved, but the oxygenation index did not improve significantly after re-checking the arterial blood gas (Table 1) D5. With the control of the patient’s condition, the patient’s blood gas analysis gradually improved. In the subsequent treatment, we continued to use HFNC for the patient for another 4 days, and gradually reduced the oxygen concentration and flow as the patient's condition improved, until the nasal cannula was used (Table 1) D10-D11. Finally, the patient's condition improved, and the patient was discharged after 17 days of hospitalization. During the whole process of HFNC oxygen therapy, the patient felt comfortable all the time and it was easy to cough up sputum in the later stage. After the patient was discharged from the hospital, we conducted a telephone follow-up. The patient had no discomfort and was competent for daily activities.
Discussion
To critically patients, the purpose of respiratory support is to maintain adequate ventilation and oxygenation, because of poor mask tolerance, however, NIV is sometimes inapplicable, then less invasive HFNC therapy gained attention as an alternative means of respiratory support [6,7]. The HFNC system is simple and can reduce the work of breathing and enhance patient comfort and tolerance [8]. It is recognized to have a number of physiological advantages, including decrease anatomical dead space, positive end-expiratory pressure effect, constant fraction of inspired oxygen, and good humidification [6]. HFNC is widely used in stable or acute exacerbation of COPD, hypoxemic respiratory failure, acute heart failure and hypercapnic respiratory failure etc, and showing some positive effects [9-13].
Among patients with acute hypoxic respiratory failure, there was no difference in intubation between HFNC and NIV, so as to mortality in patients with acute respiratory failure. Moreover, HFNC appeared to be well tolerated by patients [14,15]. This indicates that HFNC has a promising application prospect in severe patients.
On the fourth day of hospitalization, due to the aggravation of the patient's condition, the temporary change of HFNC to NIV was based on the following consideration. In the case of HFNC, the patient’s condition changed rapidly and the oxygenation index decreased significantly, suggesting that there seemed to be little benefit from continuing to use HFNC, so we chose to replace HFNC with NIV. However, the patient could not tolerate NIV and had poor coordination; the effect of assisted ventilation was not good, which was not conducive to improving the condition. Considering that the patient had clear consciousness, strong breathing muscles, and less sputum, intubation was not the best solution at the time. We finally chose to replace the ventilation equipment with HFNC again under close observation. By increasing the oxygen concentration and flow rate, it provided the patient with basic ventilation support and also improved the comfort of the patient. As far as we know, this was the first reported case of using HFNC for an oxygenation index less than 100mmHg. The timely adjustment of the treatment plan and HFNC ventilation support complement each other. Eventually, the patient avoided intubation and was cured and discharged.
To our knowledge, few studies have explored the use of HFNC in severe pneumonia solely. Tu G, et al. [16] found that there was no statistically significant difference in the ICU mortality (5% vs. 22.2%, P=.083) and the median length of the ICU stay (12 days vs. 14 days, P=0.297) between HFNC group and NIV group among renal transplant recipients secondary to severe pneumonia. However, there were fewer complications in the HFNC group (0% vs. 22.2%, P=0.042) and significantly higher of the number of ventilator-free days at day 28 (26 ± 3 vs. 21 ± 3, P < 0.001). Makino's team has applied HFNC oxygen therapy as respiratory support in their treatment of severe pneumonia and septic shock patients due to group A streptococci [17]. Kawakami N et al. also reported a case of severe mycoplasma pneumonia which used reservoir mask oxygen therapy at first, however, the patient's symptoms worsened and therefore changed to HFNC [2]. In our case, HFNC was successfully used as respiratory support to avoid discomfort in NIV and maintain oxygen saturation. Finally, the patient was discharged from the hospital.
According to our case and literature reviews, we have the following views:
1) Currently, there are few data on the use of HFNC in patients with severe pneumonia, and we hope to conduct more clinical studies in this area in the future, so as to provide more evidences for evidence-based medicine.
2) In the strict monitoring of physical signs and oxygen partial pressure, HFNC can be used for patients with severe pneumonia with low oxygenation index to avoid excessive endotracheal intubation and ventilator-associated pneumonia.
3) When using HFNC, the appropriate flow rate and inhaled oxygen fraction of the patient should be slowly titrated to avoid unnecessary replacement of respiratory support equipment.
4) For severe patients in clinical work, we need to consider both the medical effect and the patient's own comfort level to improve the patient’s compliance with treatment, so as to achieve win-win result.
Conclusion
In conclusion, HFNC seems to be a valuable respiratory support for patients with severe pneumonia. Of course, this needs more randomized controlled trials to confirm especially the comparison of advantages and disadvantages between HFNC and NIV in such patients.
References
- Brown SM, Dean NC (2011) Defining Severe Pneumonia. Clin Chest Med 32: 469-479.
- Kawakami N, Namkoong H, Ohata T (2018) A fulminant case of acute respiratory distress syndrome associated with mycoplasma pneumonia treated with nasal high-flow oxygen therapy. Case Rep Crit Care 1067593.
- Yin S (2015) Severe pneumonia in the elderly: A multivariate analysis of risk factors. Int J Clin Exp Med 8: 12463-12475.
- Mandell LA, Wunderink RG, Anzueto A (2007) Infectious Diseases Society of merica/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. Clin Infect Dis 44: S27-S72.
- Cilloniz C, Ferrer M, Liapikou A (2018) Acute Respiratory Distress Syndrome in Mechanically-Ventilated Patients with Community-Acquired Pneumonia. Eur Respir J 51: 170-215.
- Nishimura M (2015) High-flow nasal cannula oxygen therapy in adults. J Intensive Care 3: 15.
- Nishimura M (2019) High-flow nasal cannula oxygen therapy devices. Respir Care 64: 735-742.
- Ischaki E, Pantazopoulos I, Zakynthinos S (2017) Nasal high flow therapy: a novel treatment rather than a more expensive oxygen device. Eur Respir Rev 26: 17-28.
- Bonnevie T, Elkins M, Paumier C (2019) Nasal high flow for stable patients with chronic obstructive pulmonary disease: A systematic review and meta-analysis. COPD Journal of Chronic Obstructive Pulmonary Disease 16: 368-377.
- Pisani L, Astuto M, Prediletto I (2019) High flow through nasal cannula in exacerbated COPD patients: A systematic review. Pulmonol 25: 348-354.
- Lee CC, Mankodi S, Shaharyar S (2016) High flow nasal cannula versus conventional oxygen therapy and non-invasive ventilation in adults with acute hypoxemic respiratory failure: A systematic review. Respir Med 2016: 100-108.
- Huang Y, Lei W, Zhang W (2020) High-Flow Nasal Cannula in Hypercapnic Respiratory Failure: A Systematic Review and Meta-Analysis. Can Respir J: journal of the Canadian Thoracic Society 2020: 1-13.
- Clinical efficacy of high-flow oxygen therapy through nasal cannula in patients with acute heart failure 2019. J Thorac Dis 11: 410-417.
- Frat JP, Thille AW, Mercat A (2015) High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med 372: 2185.
- Monro-Somerville T, Sim M, Ruddy J (2016) The Effect of High-Flow Nasal Cannula Oxygen Therapy on Mortality and Intubation Rate in Acute Respiratory Failure: A Systematic Review and Meta-Analysis. Crit Care Med 45: e449.
- Tu G, He H, Yin K (2017) High-flow Nasal Cannula Versus Noninvasive Ventilation for Treatment of Acute Hypoxemic Respiratory Failure in Renal Transplant Recipients. Transplant Proc 49: 1325-1330.
- Hideki M, Shinji D (2017) Pneumonia and Streptococcal Toxic Shock Syndrome Due to Group A Streptococci: A Case Report. Kansenshogaku Zasshi 91: 155-158.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences