SLE Dissecting the Human Body
Saed Alnaimat, Emad Hakemi, Nadia El Hangouche and Victor Pelaez
DOI10.21767/2380-7245.100184
Saed Alnaimat1*, Emad Hakemi2, Nadia El Hangouche2 and Victor Pelaez2
1Graduate College, Rush University, Chicago, Illinois, USA
2Department of Cardiology, John H. Stroger Hospital of Cook County, Chicago, Illinois, USA
- *Corresponding Author:
- Saed Alnaimat
Graduate College
Rush University
Chicago, Illinois, USA
Tel: + (312) 864-6000
E-mail: Saed_Alnaimat@rush.edu
Received Date: June 13, 2018; Accepted Date: July 09, 2018; Published Date: July 16, 2018
Citation: Alnaimat S, Hakemi E, Hangouche NE, Pelaez V (2018) SLE Dissecting the Human Body. J Rare Disord Diagn Ther. 4:16. doi: 10.21767/2380-7245.100184
Abstract
Introduction: Aortic dissection (AD) is a rare but life threatening condition, with a cumulative mortality rate of 68% within 48 hours. Systemic lupus erythematosus (SLE) has classically been associated with heterogeneous multi-system involvement, but SLE causing AD is not well recognized. In this case, we will describe a patient with a history of SLE that presented with unique vascular complications involving major vessels.
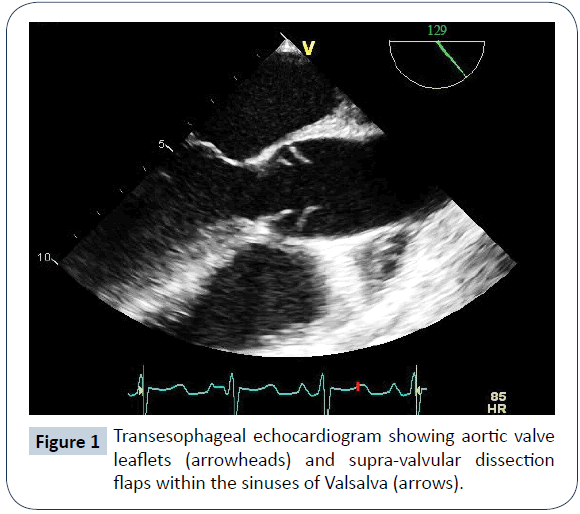
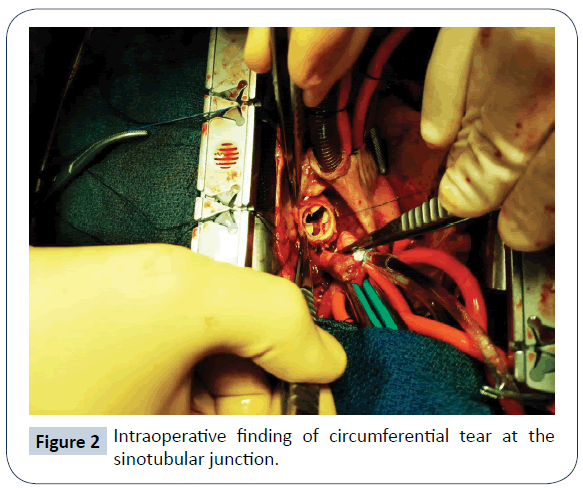
Case description: A 35-year-old female presented to emergency department with one day history of acute onset retrosternal chest pain at rest and shortness of breath. Patient had a history of SLE, lupus nephritis on hemodialysis, hypertension and chronic brachiocephalic artery dissection with extension to right carotid artery that had been managed conservatively. Her medications included hydroxychloroquine and prednisone. Further evaluation showed elevated troponins to 19 ng/mL and bilateral pulmonary edema. Echocardiography showed normal left ventricular function, new severe aortic insufficiency with possible ascending AD. Computed tomography angiogram of the aorta was inconclusive for AD. Due to high clinical suspicion, transesophageal echocardiogram was done, and showed a ring-like flap protruding into the aortic root in the vicinity of both coronary ostia, confirming ascending AD. Patient emergently underwent surgical repair of type A AD, and was found to have circumferential tear at the sinotubular junction. She had a stable hospital course.
Discussion: Review of literature reveals that AD in SLE patients is extremely rare, and only 22 cases were reported over recent years. Common features in such patients include young age, presence of systemic disease, hypertension and chronic corticosteroids use. Long-term outcomes After AD repair are still unfavorable, and patients need careful monitoring. Annual linearized mortality rate After Valve-sparing AD repair is 4.7% per year.
Keywords
Aortic dissection; Systemic lupus erythematosus; Vascular medicine; Aortic valve; Echocardiography.
Case Report
35-year-old African American female with a past medical history of SLE diagnosed 16 years ago being treated with Hydroxychloroquine and Prednisone, class IV lupus nephritis which progressed to end stage renal disease on hemodialysis, hypertension, and incidentally found brachiocephalic artery dissection with extension to right carotid artery that was managed conservatively. Patient presented with acute onset shortness of breath, retrosternal chest pain at rest, and cough with pinkish expectoration of 1 day duration. On presentation, her blood pressure was 166/41, heart rate was 108, pulse oximetry was 88% on room air, with significant respiratory distress. Auscultation revealed bilateral crackles, systolic and diastolic musical murmurs over whole precordium. Labs were noticeable for raising troponin (0.054>3.04>19), dropping hemoglobin (12.7>8.5), positive ANA (>1:160), negative dsDNA, and positive anti-RNP. Chest X-ray showed bilateral pulmonary edema. Initial bedside echo showed a vigorous LV, normal sized aortic root, but was limited due to patient’s agitation. Patient was transferred to intensive care unit for acute pulmonary edema, with possible diffuse alveolar hemorrhage. She received emergent hemodialysis, non-invasive ventilation, and nitroglycerin drip. Respiratory symptoms improved, but she continued to have recurrent chest pain that is attributed to Non-ST elevation myocardial infarction. Formal transthoracic echocardiogram (TTE) showed no regionality, but new severe aortic insufficiency with possible AD. CT angiogram of the aorta was non-conclusive by criteria for AD. Transesophageal echocardiogram (TEE, Figure 1) showed a ring-like supravalvular flap protruding into aortic valve orifice during diastole, and occluding both coronary ostia. Patient was immediately taken to operating room. Intraoperatively, patient was found to have Type A AD, with circumferential tear at the sinotubular junction (Figure 2). Patient underwent root sparing repair of type A AD with re-suspension of the commissures, and graft interposition of the dissection, and had an uncomplicated hospital course.
Discussion
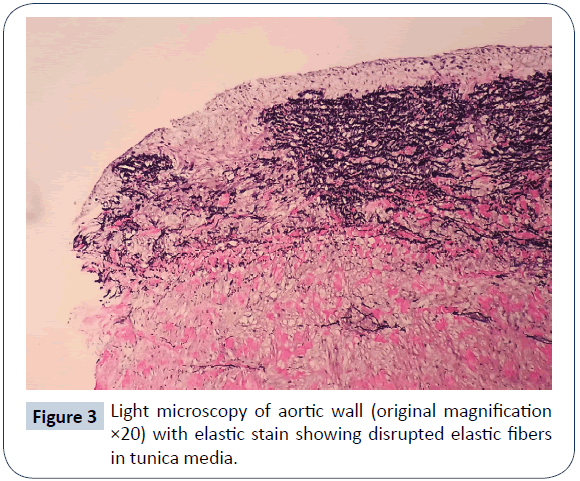
Review of literature revealed that AD in SLE patients is extremely rare, and only 22 relevant cases were reported over recent years. Common features in such patients include young age, presence of systemic disease, hypertension, and administration of corticosteroid for a long period of time [1]. Pathophysiology of AD in SLE is still unclear; suggested factors include aortitis, fibrinoid degeneration, treatment with steroids which may lead to connective tissue weakness, formation of autoantibodies against vitronectin and fibrinogen-beta, and down-regulation of the transforming growth factor beta-1 (an inhibitor of vascular wall inflammation) [2]. In our case, however, pathology reported disrupted elastic fibers in tunica media (Figure 3). Our patient had multiple vessels dissection which was attributed to underlying SLE in the setting of hypertension and corticosteroid use. She did not have any features suggestive of Marfan or Turner syndrome, or other diseases that can predispose to AD. Moreover, her hypertension was well controlled. Although CT angiography has a specificity of 98% for the diagnosis of thoracic AD [3] it did not conclusively diagnose it in our case. TEE has a comparable specificity of 95%, and was diagnostic in our case. MRI also has a specificity of 98% but it is time consuming. The estimated sensitivity of TTE for diagnosis of type A aortic syndrome remains relatively low (75-93%) despite recent advances in echocardiographic systems. Mortality rate associated with thoracic AD is high, and has recently been reported to rise by 1% to 1.4% per hour when a patient remains untreated, leading to a 68% mortality rate within 48 hours. Surgical mortality of AD repair, even in centers with a specific interest in aortic surgery, is in the range of 25% [4]. Long-term outcomes after AD repair are still unfavorable, and patients need careful monitoring. Annual mortality rate after valve-sparing AD repair is 4.7% per year [5].
Conclusion
This was a very interesting case of SLE that presented with unique and extensive vascular complications. To our knowledge, this is the first reported case of SLE complicated by circumferential AD, as well as multiple great vessel dissections involving brachiocephalic and carotid arteries. Despite that CT angiogram has a specificity of 98% for diagnosing AD, it was inconclusive in our case. This highlights the utility of TEE in diagnosis of AD, and the need for another imaging modality if the initial one was nondiagnostic.
References
- Wei HY, Chung HT, Wu CT, Huang JL (2011) Aortic Dissection Complicated with Hemothorax in an Adolescent Patient with Systemic Lupus Erythematosus: Case Report and Review of Literature. Semin Arthritis Rheum 41: 12-18.
- Sato J, Kawakami T, Nakabayashi K, Fukuoka K, Hirano K, et al. (2008) Multiple aortic aneurysms complicated by a rupture in the systemic lupus erythematosus: A case report. Pathol Res Pract 204: 845-850.
- Shiga T, Wajima Z, Apfel CC, Inoue T, Ohe Y, et al. (2006) Diagnostic Accuracy of Transesophageal Echocardiography, Helical Computed Tomography, and Magnetic Resonance Imaging for Suspected Thoracic Aortic Dissection. Arch Intern Med 166: 1350-1356.
- ACP Illinois Northern Residents ’ and Medical Students ’ Day 2016 RegOnline. 2016: 96314457.
- Saczkowski R, Malas T, Mesana T, de Kerchove L, El Khoury G, et al. (2014) Aortic valve preservation and repair in acute type A aortic dissection. Eur J Cardio-thoracic Surg 45: 220-226.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences