Rare Malignant Tumors in Mexican Pediatric Patients: A Cooperative Pediatric Oncology Research Group Report
Norma Araceli López-Facundo, Liliana Velasco-Hidalgo, Farina Esther Arreguín-González, Daniel Ortiz-Morales, Mayra López-Ruiz, Marco Rodrigo Aguilar-Ortiz , Daniela Covarrubias-Zapata, Lourdes Vega-Vega, Eduardo Jorge Baños-Rodríguez, Perla Citlali Simón-González, Isidoro Tejocote-Romero, Laura García-Segura, Cynthia Shanat Cruz-Medina, Gina Patricia De Gasperin- Estrada, Marcela Arsuaga-Jiménez M, Karen Giovana Mejía, Daniela Olvera-Caraza D and Marta Zapata-Tarrés M
DOI10.36648/2380-7245.5.2.195
Norma Araceli López-Facundo1, Liliana Velasco-Hidalgo2, Farina Esther Arreguín-González3, Daniel Ortiz-Morales4, Mayra López-Ruiz5, Marco Rodrigo Aguilar-Ortiz2, Daniela Covarrubias-Zapata6, Lourdes Vega-Vega7, Eduardo Jorge Baños-Rodríguez3, Perla Citlali Simón-González8, Isidoro Tejocote-Romero9, Laura García-Segura10, Cynthia Shanat Cruz-Medina11, Gina Patricia De Gasperin- Estrada7, Marcela Arsuaga-Jiménez M2, Karen Giovana Mejía9, Daniela Olvera-Caraza D11 and Marta Zapata-Tarrés M1*
1Hospital Materno Infantil del Instituto de Seguridad Social del Estado de México y Municipios
2Servicio de Oncología, Instituto Nacional de Pediatría
3Servicio de Oncología Pediátrica, Centro Médico Nacional 20 de Noviembre, ISSSTE Instituto de Seguridad Social y Servicio de Trabajadores del Estado
4Area de Hemato-Oncología, Hospital General de México “Dr. Eduardo Liceaga”
5Chiapas Hospital de Especialidades Pediátricas
6Centro Estatal de Oncología de Campeche “Dr. Luis González Francis”
7Hospital Infantil Teletón de Oncología, Querétaro, Mexico
8Universidad Popular del Estado de Puebla
9Hospital de Villahermosa, Tabasco
10Hospital del Niño del Instituto Materno Infantil del Estado de México
11Servicio de Pediatría, Hospital General de Celaya
12Hospital del Niño Poblano. Mexican Cooperative Pediatric Oncology research Group (SMEO) - Mexican Association of Pediatric Oncology and Hematology (AMOHP)
- *Corresponding Author:
- Marta Zapata-Tarrés
Instituto Nacional de Pediatría. Insurgentes Sur 3700 Letra C, Insurgentes Cuicuilco, 04530. Mexico City; Mexico
Tel: +5215554184099
E-mail: mzapatatarres@gmail.com
Received Date: July 19, 2018; Accepted Date: September 19, 2019; Published Date: September 26, 2019
Citation: López-Facundo NA, Velasco-Hidalgo L, Arreguín-González FE, Ortiz-Morales D, López- Ruiz M, et al. (2019) Rare Malignant Tumors in Mexican Pediatric Patients: A Cooperative Pediatric Oncology Research Group Report. J Rare Disord Diagn Ther. Vol.5 No.3:3. DOI: 10.36648/2380-7245.5.2.195
Abstract
Background: Rare malignant tumors (RMT) make up 10% of all cancer in the pediatric age. The national and international cooperative projects will allow to understand their biology and improve the treatment results, making imperative the acknowledge the clinical course and the prognosis of Mexican pediatric patients with (RMT)
Results: 178 patients were evaluated, with the age of 3 months to 17 years, 58% adolescents. The symptomatic presentation lag time was 7 days to 2 years. Most frequent symptoms were pain and palpable mass. The predominant histological type was thyroid carcinoma (29%) followed by 9% non-germ gonadal tumors and pancreatic exocrine tumors (6%). 27% metastatic. The treatment was surgical in 88%of the cases, and 5% received only palliative care. There were 38 patients with progression and 12 were due to toxicity. 18.9% of patients were lost of follow up due to abandonment of hospital care or transfer to adult hospital. Overall survival (OS) for all RMT was 63% at 100 months. SG for thyroid carcinomas was 68% within 109 months.
Conclusion: The systematic study of RMT is not possible. Patients are staged and treated with protocols designed for adults. In our series, surgery is the cornerstone of treatment. Age establishes an organizational barrier for the treatment and follow-up of these patients in our country. Nevertheless we have taken the first step for this challenge in our country by assembling the first cooperative group of rare tumors, which hopes to become a support in the clinical decisions of pediatric oncologists in Mexico.
Keywords
Rare malignancies; Children; Adolescent; Thyroid carcinoma
Abbreviations
GCIOP: Grupo Cooperativo De Investigación en Oncología Pediátrica. Cooperative Pediatric Oncology Research Group; RMT: Rare Malignant Tumors; EXPeRT: The European Cooperative Group for the Study of Rare Pediatric Tumors COG: Children´s Oncology Group
Introduction
Pediatric cancer is a rare disease in itself. In the United States of America, it is estimated that only 1% of cancer occurs in children under 20 years of age [1]. However, within pediatric cancer there are groups of diseases that usually occur infrequently and that correspond 10% to 15% of total new cases [2]. 75% of these rare malignancies occur in patients aged 15 to 19 years of age, corresponding to different histological subtypes of low incidence. They usually occur in isolation, in small numbers, without geographical association, or even at unexpected ages, which limits the understanding of their clinical and biological behavior [3]. In addition to this, these children and adolescents with RMT represent a vulnerable population that does not benefit from clinical research, as their inclusion in clinical studies is low [4]. For the majority of this type of cancer there are not systematic studies, making it difficult to know the real incidence of each histological subtype, the correct treatment, and the outcomes of those treatments, which are usually designed for adults [5]. Definition of a rare or infrequent tumor in the pediatric age is complex, and has been interpreted in different ways. The European Cooperative Group for the Study of Rare Pediatric Tumors (EXPeRT) defines them as those that have an incidence rate of 2 cases per million per year, not considered in clinical studies or both [2]. This definition emphasizes the concept of RMT is not defined only on its incidence rate but also as an orphan diseases [6,7]. The rare tumors committee of the American Children's Oncology Group (COG) includes those tumors with low prevalence in children, high incidence in adults and those of epithelial origin, in such a way that subgroup XI of the International Classification of Cancer in Children corresponds to "other malignant epithelial tumors and melanoma" and includes the histological subgroups: adrenal, thyroid, nasopharyngeal, melanoma and other unspecified carcinomas [5]. This definition does not include other rare tumors that occur almost exclusively in children, such as pancreatoblastoma and pleuropulmonary blastoma [3-7]. That been said, it requires a great effort of the collaborative groups to redefine these concepts and overcome the obstacles that have limited the study of these diseases, which will allow to generate invaluable information about the natural history of these tumors, create opportunities for their investigation and therefore offer better results [8]. Another limitation in the study of these RMTs is the low availability of biological samples for study and molecular characterization that allows defining the biological behavior and prognosis of these tumors [9-13]. The creation of cooperative groups in Europe, North and South America has managed to encourage collaborative research that includes biological samples in some rare tumors and have published their results [14-20]. They have also developed treatment recommendations for some types of cancer and identified a group of experts that supports clinical decisions. In Mexico 5.4/100,000 children under the age of 15 die annually from childhood cancer. Hence, there is an imperative need to lay the collaborative foundations to design strategies aimed at obtaining better results in the treatment of all children with cancer, including those with RMT [21]. We describe the largest multicenter cohort of pediatric patients with rare tumors in 12 Mexican centers.
Methods
We included pediatric patients with a corroborated diagnosis of childhood cancer in each of the 12 participating centers in a multicenter cohort. They were classified according to sub-section XI and XII of the International Classification of Cancer in Children, as well as considered rare in our environment as renal carcinoma and non-germ gonadal tumors [2]. We evaluated the clinical-demographic characteristics, age, gender, the main symptom and its time of evolution at diagnosis, staging according to the type of tumor. Of the variables related to the treatment, modality of treatment was gather such as, surgical, chemotherapy, radiotherapy, palliative, as well as its evolution, progression of the disease, presence of relapse, death secondary to toxicity treatment or progression of the disease and if they received palliative care treatment. Survival was evaluated in the entire group of patients, as well as survival according to each histological group. Those who dropped out of treatment and/ or were transferred to adult oncology units due to age and/ or administrative situations were excluded from the survival estimate. We performed descriptive statistics. Survival was analyzed with the Kaplan-Meier method. The data was analyzed using the software SPSS→ IBM → version number 21.
Results
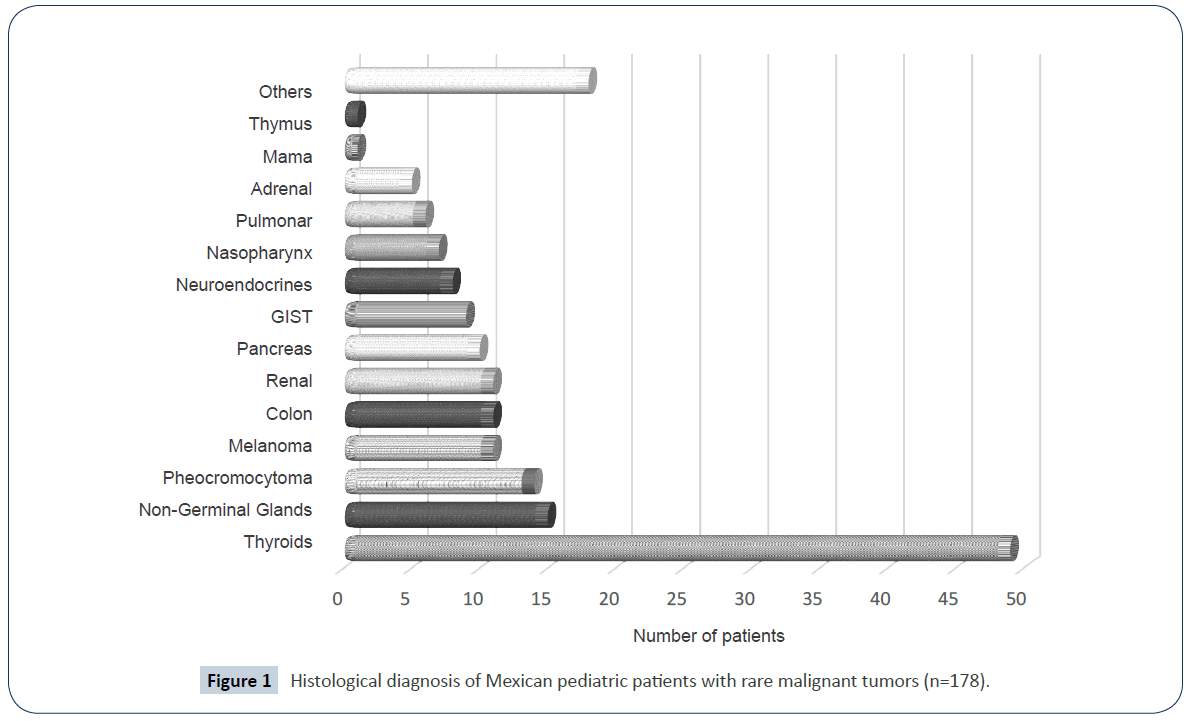
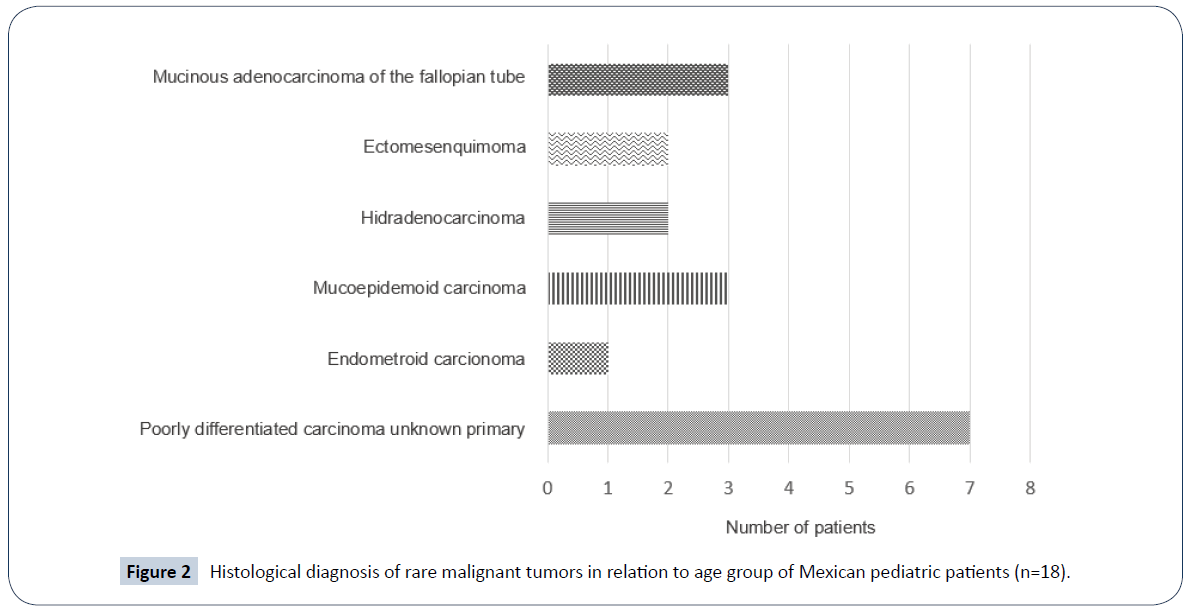
Out of a total of 5,236 new cases of childhood cancer in the 12 different hospital centers participating in our country, 178 patients were admitted to this study, they were diagnosed and treated in 12 different hospitals in the Mexican Republic during the period from January 2007 to June of 2017. The general characteristics of the patients are shown in Table 1. There were 105 women (58%) with a ratio of 1.4:1. Minimum age was 3 months and maximum of 17 years, with an average of 12 years. Patients older than 12 years old represented the 58% at the time of diagnosis, while 14% was found to be between 0 and 23 months old. The time of evolution of the symptomatology was a minimum of 7 days and a maximum of 2 years, with a median of 6 months. The most frequent symptom was pain, followed by palpable mass in some region of the economy in 18% of the cases and followed by various symptoms such as headache, precocious puberty, and jaundice. The predominant histological type was thyroid carcinoma in 49 patients (29%) followed by 9% non-germ gonadal tumors, pancreatic exocrine tumors, melanoma and colon carcinoma (6%). The frequency distribution of RMT is shown in Figure 1. Also within this classification we observed a group of 18 patients with tumors considered rare among the RMT corresponding to poorly differentiated carcinomas of unknown primary and malignant tumor of the sweat gland Figure 2. Regarding the distribution of frequencies by age group it was observed that renal carcinomas and sarcomas predominated in patients younger than 24 months, whereas in toddlers and adolescents, thyroid carcinomas and non-germ gonadal tumors predominated, being the most frequent granulose tumor Table 2. In 28% of the patients presented metastatic disease at diagnosis and/or bulky tumors.
| Characteristics | N 178 (%) |
|---|---|
| Gender | |
| Female | 105 (59%) |
| Male | 73 (41%) |
| Age (months) | |
| 0-24 | 25 (14%) |
| 25-60 | 15 (8%) |
| 61-120 | 35 (20%) |
| ≥ 121 | 103 (58%) |
| Main symptoms | |
| Mass, pain and/or distension in abdomen Mass in other places | 54 (30%) |
| Pain in other places | 47 (26%) |
| Cephealea Precocious | 15 (8%) |
| Puberty Persistent | 15 (8%) |
| Vomiting | 11 (6%) |
| High Blood Pressure | 10 (5%) |
| Gastrointestinal bleeding | 6 (3%) |
| Seizures | 6 (1%) |
| Hypocalcemia | 3 (1%) |
| Other Symptoms | 8 (4%) |
| Histologic grade | |
| I | 20 (11%) |
| II | 42 (23%) |
| III | 54 (30%) |
| IV | 50 (29%) |
| Undertermined* | 12 (7%) |
*Due to early death
Table 1: General characteristics of Mexican pediatric patients with rare malignancies.
| Age Group (Months) | Number Patients (%) | Most frequent histological diagnostics |
|---|---|---|
| 0-24 m | 25 (14%) | Renal, adrenal |
| 25-60 m | 15 (8%) | Neuroendocrines tumors |
| 61-120 m | 35 (20%) | Non Germinal ovarian tumors/Thyrod |
| ≥ 121 m | 103 (58%) | Thyrod carcinoma, Non germinal ovarian cancer, Others |
Table 2: Histological diagnosis of rare malignant tumors in relation to age group in Mexican pediatric patients (n=178).
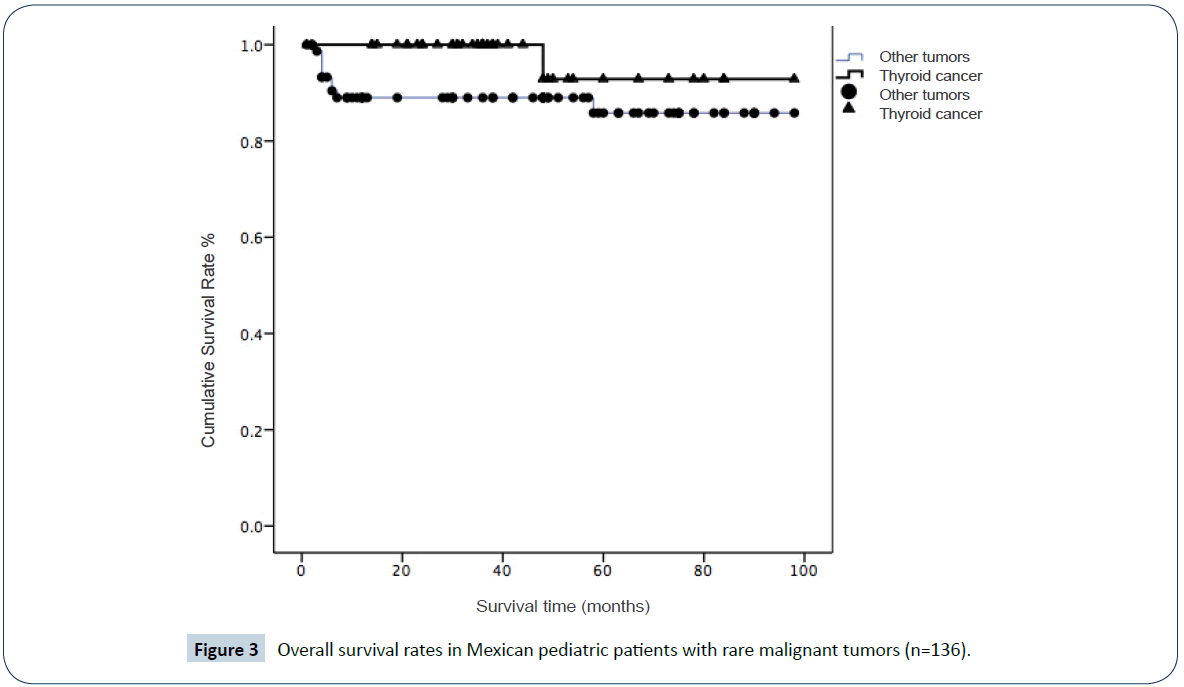
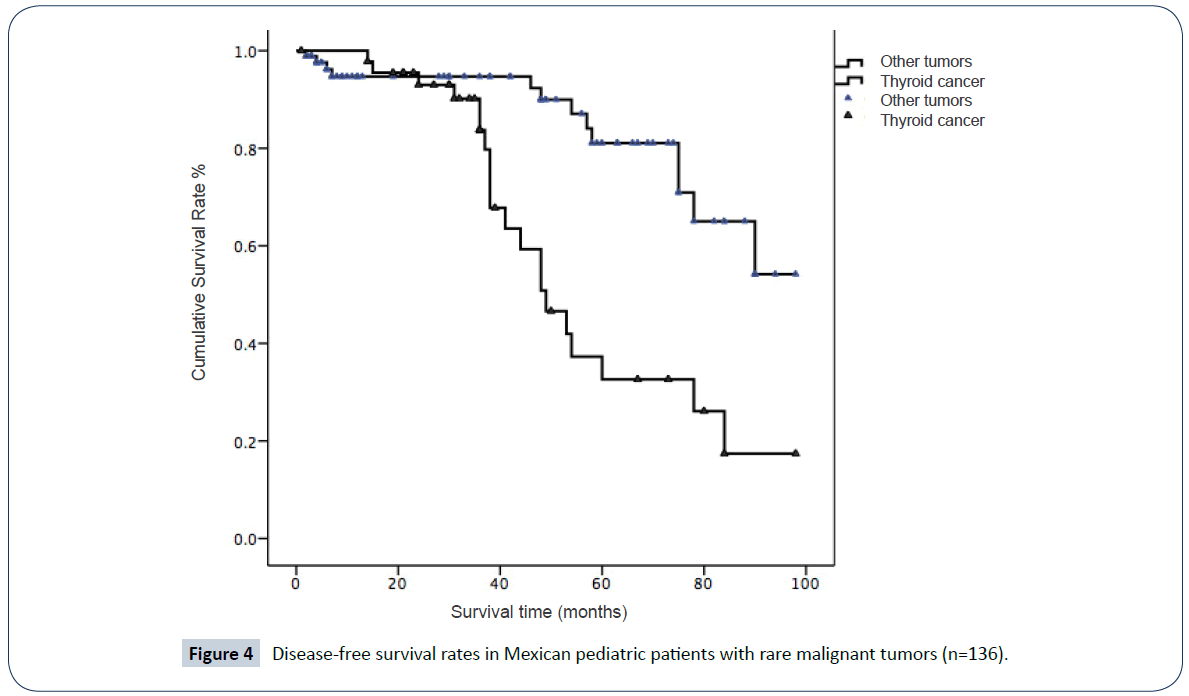
The predominant initial treatment was surgery in 91% of patients; in 10% of cases with surgeries were performed at different times. 3% received only palliative care treatment from the moment of diagnosis due to illness considered incurable Table 3. In 19% of patients the follow-up was lost due to treatment abandonment due to social reasons or transfer to an adult oncology unit, since in Mexico health institutions limit the pediatric age to 15, 16 or 18 years-old. Therefore the administration cannot continue their care in pediatric hospitals. Relapse and/or progression of the disease was documented in 33 of the 136 evaluable patients for survival (24%), 20 of them had thyroid carcinomas. We registered 33 deaths, 21 of them in patients with previous treatment abandonment who re-entered the program with progressive disease, 8 died because of disease progression and 4 because of treatment toxicity or surgical complications. The overall survival (OS) for the entire series of patients with RMT was 91% at 88 ± 2.5 months (95% CI 95-93). Likewise, survival was estimated at 97% at 94 ± 3.4 months (95% CI 87-101) for thyroid carcinoma and 87% at 85 ± 3.5 months 95% CI 77-93) p 0.05 (Figure 3). Disease-free survival forpatients with thyroid carcinoma was 56% at 82 ± 3 months (95% CI 75-89) while for the rest of the RMT it was 85% at 57± months (95% CI 47-67) p=0.001 (Figure 4).
| Modality used | Number of patients (%) |
|---|---|
| Surgery | 163 (91%) |
| Quimiotherapy | 77 (43%) |
| Radiotherapy | 35 (20%) |
| Palliative care only | 16 (3%) |
| Surgery + Quimiotherapy | 69 (38%) |
| Surgery + Quimiotherapy + Radiotherapy | 20 (11%) |
| Paliative care due to desease progression | 18 (10%) |
| Treatment abandonment | 30 (16.8%) |
| Transfer to Adult Unit during treatment /follow-up | 12 ( 7% ) |
| Death after treatment abandonment | 21 (12 %) |
Table 3: Therapeutic modalities used in Mexican pediatric patients with rare malignancies (n=178).
Discussion
Childhood cancer by definition, is a rare disease. The RMT represents 15% of all malignant neoplasms in children under the age of 20. 30% of the cases occur between the ages of 15 to 19 according to reports from the Children´s Oncology Group [22]. For example, Germany reported 232 cases from 2001 to 2012; Turkey 43 of 579 from 2002 to 2012 [23-25] and also, the South American group reported a series of 276 cases from 2000 to 2005 [9]. Likewise, series have been reported in France and Poland. This report is a case series of 10 years in collaboration with 12 hospitals in Mexico. The most frequent rare tumor was thyroid carcinoma in its different varieties, followed by non-germ gonadal tumors, and in this series we reported 16 patients with rare tumors within the Rare Malignant Tumors Corresponding to group XI and XII of the international classification of the child cancer [5]. One limitation of this serie is that a histopathological concordance study of all tumors was not performed in all the participating centers. Another limitation of our series is that we do not have the genetic and molecular characterization associated with some rare tumors such as pleuropulmonary blastoma, medullary carcinoma of the thyroid, carcinoma of the colon, etc. [26-32]. Although in our country the majority of our patients with childhood cancer are diagnosed with advanced disease and it is not different for patients with RMT who are usually diagnosed with bulky masses and mostly with metastatic disease. Late diagnosis and transfer to an oncology center are common problems despite the efforts made by health institutions; this phenomenon can be attributable to multiple sociocultural circumstances and organizational barriers that limit access to early diagnosis [33-35]. In relation to the treatment of pediatric patients with RMT, surgery is the cornerstone of treatment, especially in patients with resectable tumors. Pediatric surgical oncologists operate pediatric patients with thyroid carcinoma frequently. Likewise, patients with large abdominal masses are submitted only to a biopsy and/or to the resolution of a compressive oncological emergency, especially at the abdominal or spinal level. The therapeutic protocols were those that are usually used in adult patients. Only 5% of patients received palliative care treatment from the time of diagnosis. Multiple circumstances can influence the decision of the pediatric oncologist to initiate palliative care at diagnosis [36- 38]. However, in a country where resources are very limited and access to innovative treatments is a luxury, achieving the disease control with the resources available in a patient with a bad prognosis could be considered as a true success. Radiotherapy in most of our patients was considered an important therapeutic modality despite the toxicity involved. Prognosis of all patients in this series does not seem to be so dismal, however survival rate is based on the number of patients with thyroid carcinomas that compared with adults as they have quite an acceptable long-term survival as well as in series reported [39]. The complete analysis of the treatment and survival rate of pediatric patients with thyroid carcinomas is the subject of a new study for our group. The number of patients who drop out of treatment mainly due to sociocultural situations, as described in other countries [40,41]. Although, age represents an organizational barrier for the treatment and follow-up of these patients since for administrative reasons, in Mexico, they must be transferred to adult hospitals. Officially, adulthood begins at 18 years of age and the pediatric age varies from one institution to another, and a patient can be considered as an adult from 15 years and 0 days of age, which limits administratively the possibility of starting a treatment, complete it or have a long-term follow-up. This has also been considered as a reason for treatment abandonment [42].
Conclusion
Rare tumors are a real challenge for the pediatric oncologist. The cooperative groups are an invaluable resource for pediatric oncology, generate information of vital importance and guarantee the quality of attention to the children. We have taken the first step for this challenge in our country by integrating the first cooperative group of rare tumors, which hopes to become a support group in the clinical decisions of pediatric oncologists in Mexico.
References
- Siegel R, Ma J, Zou Z, Jemal A (2014) Cancer statistics, 2014. CA Cancer J Clin 64: 9-29.
- Bisogno G, Ferrari A, Bien E, Brecht I, Brennan B, et al. (2012) Rare cancers in children: The EXPeRT initiative—A report from the European Cooperative Study Group on Pediatric Rare Tumors. Klin Padiatr 224: 416-420.
- Pappo AS, Krailo M, Chen Z, Rodriguez-Galindo C, Reaman G, et al. (2010) Infrequent tumor initiative of the Children’s Oncology Group: Initial lessons learned and their impact on future plans. J Clin Oncol 28: 5011-5016.
- Shaw PH, Hayes-Lattin B, Johnson R (2014) Improving enrollment in clinical trials for adolescents with cancer. Pediatrics 133: 109-113.
- https://seer.cancer.gov/csr/1975_2007/results_merged/sect_29_childhood_cancer_iccc.pdf
- Ferrari A, Bisogno G, De Salvo GL, Indolfi P, Perilongo G, et al. (2007) The challenge of very rare tumors in childhood: The Italian TREP project. Eur J Cancer 43: 654-659.
- Harms D, Schmidt D (1993) Rare tumors in childhood: pathological aspects. Experience of the Kiel Pediatric Tumor Registry. Med Pediatr Oncol 21: 23 9-48.
- Keat N, Law K, McConnell A, Seymour M, Welch J, et al. (2013) International rare cancers initiative (IRCI) Ecancermedicalscience 7: 20.
- Villarroel M, Chantada LG (2015) Tumores raros en adolescentes. Rev Med Clin Condes 26: 495-502.
- Kamartsubara K, Carvajal R (2016) The promise and challenges of rare cancer research. Lancet Oncol 17: 136-138.
- Boyd Niki, Dancey J, Blake G (2016) Rare cancers: a sea of opportunity. Lancet Oncol 17: 52-61.
- Kotecha R, Kees V, Cole C (2015) Rare childhood cancers an increasing entity requiring the need for global concensus and collaboration. Cancer Med 6: 819-824.
- Pilla R (2017) Rare cancers: Challenges and issues. Indian J Med Res 45: 17- 27.
- Hill DA, Furman WL, Billups CA, Riedley SE, Cain AM, et al. (2007) Colorectal carcinoma in childhood and adolescence: a clinicopathologic review. J Clin Oncol 25: 5808-5814.
- Sultan I, Rodriguez-Galindo C, El-Taani H, Pastore G, Casanova M, et al. (2010) Distinct features of colorectal cancer in children and adolescents: a population-based study of 159 cases. Cancer 116: 758-765.
- Wong JR, Harris JK, Rodriguez-Galindo C, Johnson KJ (2013) Incidence of childhood and adolescent melanoma in the United States: 1973-2009. Pediatrics 131: 846-854.
- Ayan I, Kaytan E, Ayan N (2003) Childhood nasopharyngeal carcinoma from biology to treatment. Lancet Oncology 4: 13-21.
- Messinger YH, Stewart DR, Priest JR, Williams GM, Harris AK, et al. (2015) Pleuropulmonary Blastoma: A Report on 350 Central Pathology–Confirmed Pleuropulmonary Blastoma Cases by the International Pleuropulmonary Blastoma Registry. Cancer 121: 276-285.
- Ribeiro RC, Pinto EM, Zambetti GP, Rodriguez-Galindo C (2012) The International Pediatric Adrenocortical Tumor Registry initiative: Contributions to clinical, biological, and treatment advances in pediatric adrenocortical tumors. Mol Cell Endocrinol 351: 37-43.
- Bisogno D, Brennan B, Orbach D (2014) Treatment and prognostic factors in Pleuropulmonary blastoma: An expert report. Eur J Cancer 50: 178-84.
- https://censia.salud.gob.mx/contenidos/descargas/cancer/20160601_Boletin- 2014_SEDP12sep16_4.pdf
- https://rarediseases.info.nih.gov/RareDiseaseList.aspx
- Brecht IB, Bremensdorfer C, Schneider DT, Frühwald MC, Offenmüller S, et al. (2014) Rare malignant pediatric tumors registered in the German Childhood Cancer Registry 2001-2010. Pediatr Blood Cancer 7: 1202-1209.
- Brecht IB, Graf N, Schweinitz DV, Fruhwald MC, Bielack SS, et al. (2009) Networking for children and adolescents with very rare tumors: foundation of the GPOH Pediatric Rare Tumor Group. Klin Padiatr. 221: 181-185.
- Özyörük D, Yavuz G, Dinçaslan H, Tanyıldız G, Tacylidiz N, et al. (2013) Rare childhood tumors in a Turkish prediatric oncology center. Indian J Med Pediatr Oncol 4: 264.
- Bien E, Stachowicz-Stencel T, Godzinski J, Balcerska A, Izycka-swieszewska E, et al. (2009) Oncological Centers of the Polish Pediatric Solid Tumors Study Group. Retrospective multi-institutional study on heman- giopericytoma in Polish children. Pediatr Int 51: 19-24.
- Reguerre Y, Lacour B, Andre N, Claude L, Hameury F, et al. (2010) Epidemiology and management of rare paediatric tumours within the framework of the French Society for Children Cancer. Bull Cancer 97: 1041-1045.
- Pugh TJ, Yu W, Yang J, Field AL, Ambrogio L, et al. (2014) Exome sequencing of pleuropulmonary blastoma reveals frequent biallelic loss of TP53 and two hits in DICER1 resulting in retention of 5p-derived miRNA hairpin loop sequences. Oncogene 33: 5295-5302.
- Figueiredo BC, Sandrini R, Zambetti GP, Pereira RM, Cheng C, et al. (2006) Penetrance of adrenocortical tumours associated with the germline TP53 R337H mutation. J Med Genet 43: 91-96.
- Chau NG, Mitchell CM, Aserlind A, Grunfeld N, Kaplan L, et al. (2014) Aggressive treatment and survival outcomes in NUT midline carcinoma (NMC) of the head and neck (HN). J Clin Oncol 32: 6057.
- Dall’igna P, Cecchetto G, Bisogno G, Conte M, Chiesa PL, et al. (2010) Pancreatic tumors in children and adolescents: the Italian TREP project experience. Pediatr Blood Cancer 54:675-680.
- Pinto EM, Ribeiro RC, Figueiredo BC, Zambetti GP (2011) TP53 associated pediatric malignancies. Genes Cancer 2: 485-490.
- Pashankar F, Rodriguez-Galindo C, Pappo A (2012) Development of a therapeutic approach to rare cancers in children: The Children’s Oncology Group Experience. J Pediatr Hematol Oncol 34: 37-38.
- Ramirez-Ortiz MA, Ponce-Castañeda MV, Cabrera-Muñoz ML, Medina-Sanson A, Liu X, et al. (2014) Diagnostic delay and sociodemographic predictors of stage at diagnosis and mortality in unilateral and bilateral retinoblastoma. Cancer Epidemiol Biomarkers Prev 23: 784-792.
- Fajardo-Gutierrez A, Sandoval-Mex AM, Mejia-Arangure JM, Rendón-Macías ME, Del Martínez-García MC, et al. (2002) Clinical and social factors that affect the time to diagnosis of Mexican children with cancer. Med Pediatr Oncol 39: 25-31.
- De Lacerda AF, Gomez B (2017) Trends in case and place of death for children in Portugal (a European country with no paediatric palliative care during 1987-2011: A population-based study. BMC Pediatr 17: 215.
- Day EJ, Langner R, Stirling LC, Hough R, Bluebond-Langner M, et al. (2018) We just follow the patients' lead": Healthcare professional perspectives on the involvement of teenagers with cancer in decision making. Pediatr Blood Cancer 65: e26898.
- Thrane SE, Maurer SH, Cohen SM, May C, Sereika SM, et al. (2017) Pediatric Palliative Care: A five-year retrospective Chart Review Study. J Palliat Med 20: 1104-1111.
- Pan JJ, Zhao L, Cheng R, Yang Y, Hu YH, et al. (2017) Thyroid carcinoma in children and adolescents: Clinical characteristics and follow-up from two centers. J Can Res Ther 13: 715-719.
- Friedrich P, Lam CG, Kaur G, Itriago E, Ribeiro RC, et al. (2007) Determinants of treatment abandonment in childhood cancer. Results from a Global Survey. PLoS One 10: e0163090.
- Gupta S, Yeh S, Martiniuk A, Lam CG, Chen HY, et al. (2013) The magnitude and predictors of abandonment of therapy in paediatric acute leukaemia in middle-income countries: A systematic review and meta-analysis. Eur J Cancer 49: 2555-2564.
- Künder-Klünder M, Miranda-Lora AL, Dorantes Acosta E, Zapata-Tarrés M, Carranco-Hernández T, et al. (2012) Treatment abandonment in pediatric patients with acute lymphoblastic leukemia. Bol Med Hosp Infant Mex 69: 226-232.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences