Long Term Response of a Patient with Lymphangiomatosis under Bevacizumab Therapy- A Case Report
Sotirios Sachanas*, Gerassimos A. Pangalis, Anastasios Koutsopoulos, Panagiotis Kekis, Dimitrios Tsamis, Chrysothea Zaroulis, Efstathios Koulieris, Maria Moschogiannis, Xanthi Yiakoumis and Ioannis Anastasakis
1Department of Haematology, Athens Medical Center-Psychikon Branch, Athens, Greece
2Laboratory of Pathology, University Hospital of Heraklion, Heraklion, Crete, Greece
3Department of Surgical, Athens Medical Center-Psychikon Branch, Athens, Greece
4Department of Radiology, Athens Medical Center-Psychikon Branch, Athens, Greece
- *Corresponding Author:
- Sotirios Sachanas
Department of Haematology
Athens Medical Center-Psychikon Branch
Andersen 1, N. Psychikon 11525, Athens, Greece
E-mail: ssachanas@gmail.com
Received Date: June 23, 2020; Accepted Date: July 16, 2020; Published Date: July 23, 2020
Citation: Sachanas S, Pangalis GA, Koutsopoulos A, Kekis P, Tsamis D, et al. (2020) Long Term Response of a Patient with Lymphangiomatosis under Bevacizumab Therapy: A Case Report. J Rare Disord Diagn Ther Vol.6 No.5:9. DOI: 10.36648/2380-7245.6.5.206
Abstract
Lymphangiomatosis is a rare disorder that affects multiorgan: cyst formation due to lymphatic channel increase and increased permeability causes various symptoms. Its optimal treatment strategy is yet to be determined. Lymphatic vessel proliferation is regulated by the expression of the signal protein Vascular Endothelial Growth Factor (VEGF) and its subtypes and monoclonal antibodies targeting this factor have been used in the treatment of several human tumors. Since lymphangiomatosis is also due to abnormal lymphatic vessel proliferation, we hypothesized that anti-angiogenic agent Bevacizumab may also be effective in this lymphatic disorder. Here, we report a male patient with lymphangiomatosis: Bevacizumab successfully ameliorated generalized edema and multiple massive lymphatic cysts. Although experience of one case does not lead in definitive results, we suggest that Bevacizumab may be an option for intractable cases of lymphangiomatosis.
Keywords
Lymphangiomatosis; Lymphatic cysts; Bevacizumab; Edema; Albumin
Introduction
Lymphangiomatosis is a multi-system disorder and is thought to be the result of congenital errors of lymphatic development occurring prior to the 20th week of gestation, characterized by the presence of cysts that result from an increase both in the size and number of thin-walled lymphatic channels [1,2]. Symptoms depend on the organ system involved and to the extent of the disease while it is possible patients especially early in the course of the disease to be asymptomatic [3]. Different therapies have been applied in patients with lymphangiomatosis but there are no standardised treatment protocols or guidelines for these patients. Due to the rarity of the disease various treatments have been administered mainly as part of single case reports [4-8]. In recent years, much has been learned about the stimulators and inhibitors of lymphangiogenesis and members of VEGF family have emerged as prime mediators of this process [9,10] while there have been also few cases on Bevacizumab successfully treated patients with lymphangiomatosis [6,7]. The latter comprises a monoclonal antibody that binds to VEGF resulting in inhibition of angiogenesis and it is used mostly in patients with solid tumors [11]. Here, we report a case of a patient with lymphangiomatosis with a delayed onset of symptoms who presented with massive lymphatic cysts both in thorax and abdomen and concomitant generalized edema treated successfully with Bevacizumab remaining up to now after 3 years from therapy initiation on treatment with ongoing response and decrease of the disease “burden” with reduction of the size of cysts.
Case Report
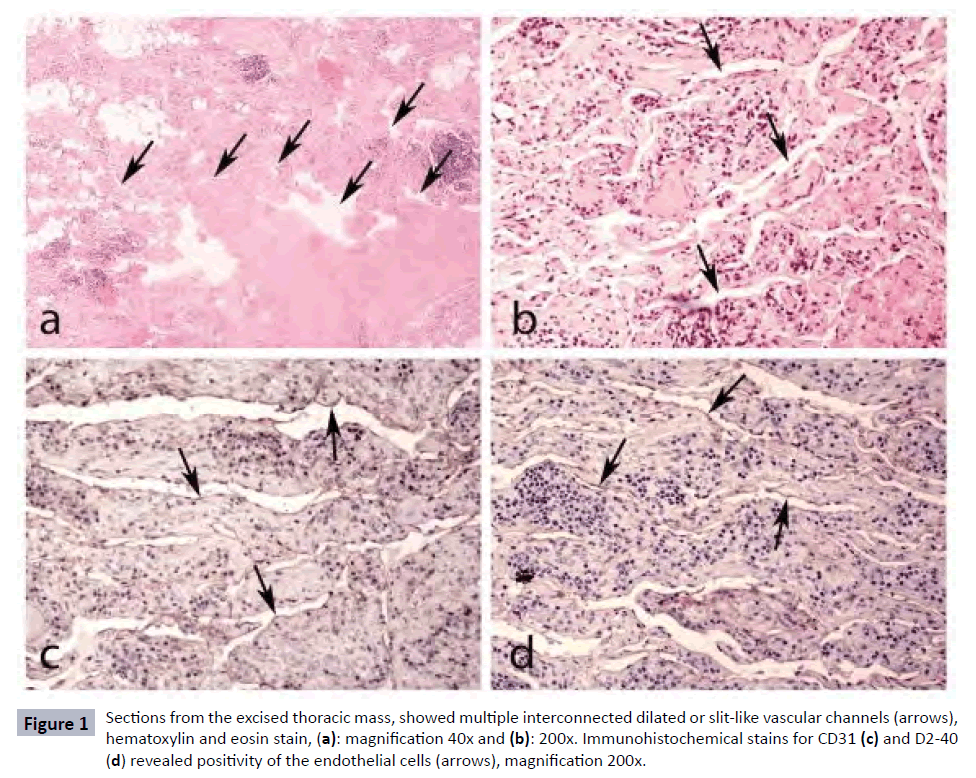
A 54-year-old male was diagnosed with lymphangiomatosis at the University Hospital of Heraklion, in Crete, where he lived permanently, on May 2016. Three months earlier while asymptomatic he underwent a thorax and abdomen computed tomography (CT) evaluation due to the suspicion of an aorta aneurysmatic enlargement in a thorax x-Ray assessment. CT evaluation revealed the presence of multiple cystic-like lesions forming locally excessive masses without enhancement with fluid density distributed in both the paraortic areas, the biggest of which reached 12cm. Multiple similar lesions were found in the peritoneal and retroperitoneal space, the biggest of which reached 22cm. A laboratory examination for tuberculosis was negative and other blood laboratory tests were normal. Subsequently, a CT guided biopsy of the thoracic mass was performed which was no diagnostic and thereafter a laparoscopic biopsy of an abdominal mass was performed which was also inconclusive. He underwent also a bone marrow aspiration plus biopsy which did not reveal abnormal findings. Eventually, a surgical excision of a right thoracic mass was performed the biopsy of which disclosed findings macroscopically consistent with lymphangiomatosis. Histopathology showed fibro-adipose tissue with an increased number of dilated and slit-like anastomosing lymphatic vessels, lined by a single layer of flattened endothelial cells, without atypia (absence of endothelial tufting or mitotic activity). Endothelial cells showed positivity for the immunohistochemical markers CD31 and D2-40 (antibody which recognizes the specific transmembrane protein, podoplanin, expressed by lymphatic cells) (Figure 1) [12], findings consistent with the diagnosis of lymphangiomatosis. His diagnostic work-up included also an upper and lower gastrointestinal tract assessment which showed the presence of duodenal lymphangiectasia. Thus, our patient was placed under close monitoring and under a specific nutrition based on median chain triglycerides. He was referred to our Department on October 2016 for consultation. He was clinically fit and physical examination did not reveal anything apart from a decrease of the respiratory murmur in the right lower pulmonary site where a thoracic biopsy had been performed. Laboratory tests indicated a slight decrease of B12 levels and low albumin levels (2.1 mg/dl) and he was advised to continue the dietary program.
Figure 1: Sections from the excised thoracic mass, showed multiple interconnected dilated or slit-like vascular channels (arrows), hematoxylin and eosin stain, (a): magnification 40x and (b): 200x. Immunohistochemical stains for CD31 (c) and D2-40 (d) revealed positivity of the endothelial cells (arrows), magnification 200x.
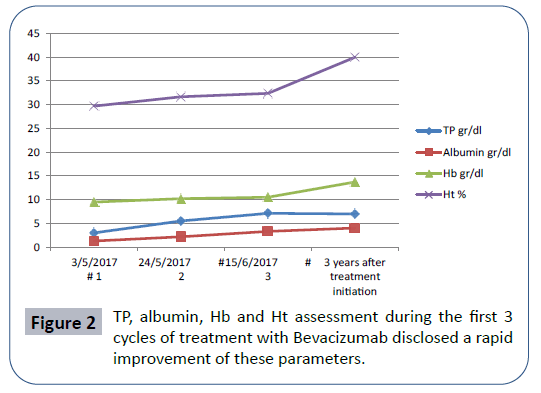
He was admitted again to our Department five months later because of deterioration of his physical condition. Upon his admission on May 2017 he was presented with generalized edema particularly at the lower extremities. Due to the excessive leg edema he could not walk easily and there was a need for an escort to provide him assistance while he was pale with shortness of breath. His blood cell counts showed: white blood cell (WBC): 9.83 × 109/l, lymphocytes: 0.26 × 109/l, granulocytes: 9.36 × 109/l, hemoglobulin (Hb): 9.6 g/dl, hematocrit (Ht): 29.1%, platelets: 391 × 109/l. Anemia was normocytic normochromic, hemolysis indices were negative and there was not any blood loss. Biochemical examination revealed a significant decrease of Total Proteins (TP) and albumin levels (3.5 g/dl and 1.3 g/dl respectively). Thorax and abdomen CT evaluation demonstrated apart from the known excessive cystic lesions the presence of pleural and peritoneal fluid. Thus, we decided except of the supportive care to proceed to treatment for the underlying lymphangiomatosis. Taking into consideration the fact that the angiogenic factor VEGF is implicated in lymphatic proliferation as well as the fact that there were a few reports on patients treated with the anti-angiogenic agent Bevacizumab our patient was placed on the aforementioned agent, at a dose of 1 mg/ kg intravenously, every 3 weeks. After one cycle our patient demonstrated clinical and laboratory response with:
1. Decrease of edema at lower extremities,
2. Elevation of TPs and albumin levels,
3. Improvement of anemia (Figure 2),
4. Slight decrease of the masses both in thorax and abdomen as well as disappearance of pleural and peritoneal fluids.
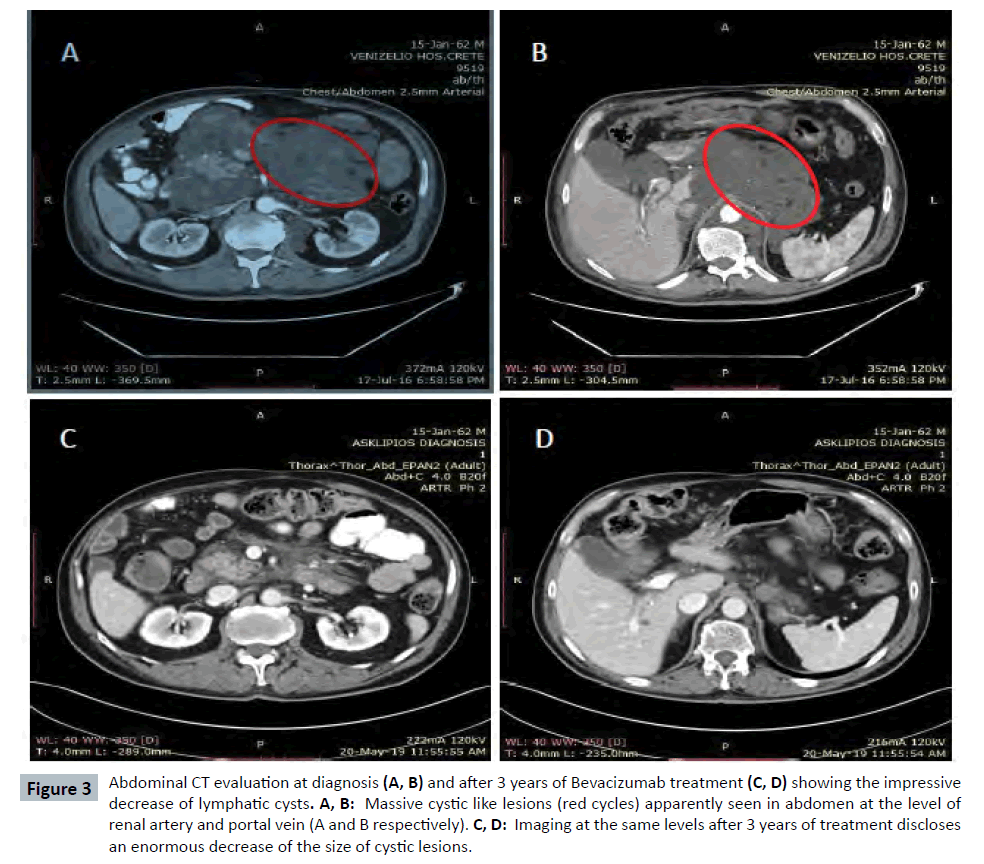
After almost 3 years our patient continues to be on Bevacizumab with good tolerance and without side effects. There was only a need for a temporal interruption of therapy in order a purulence of a cyst at right ileac site to be surgically managed. Currently he is in good clinical condition and he continues his daily activities including his job. His last laboratory exams showed Ht: 40%, Hb: 13.7 mg/dl, TP: 7 g/dl, albumin: 4.05 g/dl (Figure 2 and Table 1) and the consecutive CT evaluation demonstrated a continuing decrease of cystic lesions (Figure 3).
Figure 3: Abdominal CT evaluation at diagnosis (A, B) and after 3 years of Bevacizumab treatment (C, D) showing the impressive decrease of lymphatic cysts. A, B: Massive cystic like lesions (red cycles) apparently seen in abdomen at the level of renal artery and portal vein (A and B respectively). C, D: Imaging at the same levels after 3 years of treatment discloses an enormous decrease of the size of cystic lesions.
| Date of treatment #cycles | TP gr/dl | Albumin gr/dl | Hb gr/dl | Ht % |
|---|---|---|---|---|
| 03/05/17Ãâà#1 | 3 | 1,3 | 9,5 | 29,7 |
| 24/05/17Ãâà#2 | 5,5 | 2,2 | 10,2 | 31,7 |
| 15/6/17Ãâà#3 | 7,1 | 3,3 | 10,5 | 32,4 |
| 3 years from treatment initiation | 7,0 | 4,05 | 13,7 | 40 |
Table 1: Three years from treatment initiation there is an ongoing response.
Discussion
Lymphangiomatosis describing the presence of multiple lymphangiomas is a very rare disease entity characterized by lymphatic malformation consisting of variously dilated lymphatic channels or cysts, lined by endothelial cells with a lymphatic phenotype [13]. Recently, lymphangiomatosis has been renamed as generalized lymphatic anomaly (GLA) by the International Society for the Study of Vascular Anomalies (ISSVA) in the updated classification of vascular anomalies [14]. GLA is defined as a multifocal lymphatic malformation that may affect the skin and superficial soft tissue as well as abdominal and thoracic viscera and often involve bones while chylous effusions at various anatomical sites (pericardial, pleural, or peritoneal) may be present [14]. It usually presents in childhood but can also be diagnosed in adults and seems to have no sex predilection [15]. Symptoms depend on the organ system involved and also on the extent of the disease. Patients could be asymptomatic for many years but over time the abnormally proliferating lymphatic channels that constitute lymphangiomatosis are capable of massive expansion and infiltration into surrounding tissues, bone, and organ causing various clinical manifestations [1,2].
Of note was the fact that our patient was asymptomatic up to age of 54. The presentation of lymphangiomatosis at a later age could be attributed to the influence of hormonal factors or could be represent a specific type of disease that is more subtle and widespread requiring a longer time for growth [2]. In our case, patient’s condition was deteriorated approximately one year after the diagnosis mainly due to the severe decline of albumin levels resulting in generalized edema. This excessive loss of proteins could be attributed to intestinal lymphangiectasia resulting in impaired integrity of the mucosa [16]. Literature review demonstrated that due to the rarity of the disease there are no standardised treatment protocols or guidelines for these patients. Treatment has been limited to surgical resection or drainage procedures in case of limited lymphangiomas whereas sclerotherapy with various agents such as the streptococcus antigen OK-432 or doxycycline has been an additional treatment option for patients with non-extended disease [17-19]. Radiation therapy has been applied in patients with an extensive disease at the cost of radiation-related pneumonitis [20]. Systemic therapy with various agents such as interferon, propranolol, a nonselective b-blocker, and more recently sirolimus, a mammalian target of rapamycine inhibitor, have been used in patients with generalized lymphatic malformations [4,5,21-23]. The latter has been used mostly at a pediatric population while Ozeki et al. has been published recently data from a series of twenty patients with median age of 16 years (range:2 weeks-55years) diagnosed with a variety of lymphatic anomalies and heterogeneous disorders treated with sirolimus with promising results [8,21-23]. Moreover, one case of bilateral lung transplantation has been reported [24]. Finally, dietary treatments, such as total parenteral nutrition, medium-chain triglycerides and high-protein diets, have generally proven to be ineffective as such in our case. On the other hand it has been reported that lymphatic vessel proliferation is influenced by the expression of a signal protein, namely VEGF and its subtypes and monoclonal antibodies targeting this factor have been approved for clinical use in the treatment of several human tumors [9,10,25,26]. Based on this rationale the anti-angiogenic factor Bevacizumab has been successfully given in some cases including a child who suffered by multifocal lymphangiomatosis receiving Bevacizumab for a long time at a dose of 10 mg/kg every month and an adult with diffuse pulmonary lymphangiomatosis who received Bevacizumab at a dose of 1 mg/kg, every three weeks for only 7 cycles due to Bevacizumab-related side effects.
Conclusion
To our knowledge our patient is the only adult patient with lymphangiomatosis who has such a prolonged response still under Bevacizumab reaching 36 months without any particular side effect with an ongoing decrease of the dimensions of the cystic lesions. Bevacizumab way of administration was based on the experience in patients with solid tumors who receive this agent continuously until disease progression or until unacceptable toxicity. This case report showed in line with previous reports that Bevacizumab is a feasible and highly effective therapy for intractable cases of lymphangiomatosis. Moreover, the continuing decrease of lymphatic cysts may be attributed to the prolonged administration of Bevacizumab reflecting its unique mechanism of action.
Conflict of Interest
None.
References
- Marom EM, Moran CA, Munden RF (2004) Generalized lymphangiomatosis. Am J Roentgenol 182: 1068.
- Faul JL, Berry GJ, Colby TV, Ruoss SJ, Walter MB, et al. (2000) Thoracic lymphangiomas, lymphangiectasis, lymphangiomatosis, and lymphatic dysplasia syndrome. Am J Respir Crit Care Med 161: 1037-1046.
- Luisi F, Torre O, Harari S (2016) Thoracic involvement in generalised lymphatic anomaly (or lymphangiomatosis). Eur Respir Rev 140: 170-177.
- Laverdiere C, David M, Dubois J, Russo P, Hershon L, et al. (2000) Improvement of disseminated lymphangiomatosis with recombinant interferon therapy. Pediatr Pulmonol 29: 321-324.
- Ozeki M, Fukao T, Kondo N (2011) Propranolol for intractable diffuse lymphangiomatosis. N Engl J Med 364: 1380-1382.
- Aman J, Thunnissen E, Paul MA, van Nieuw Amerongen GP , Vonk-Noordegraaf A, et al. (2012) Successful treatment of diffuse pulmonary lymphangiomatosis with bevacizumab. Ann Intern Med 156: 839-840.
- Grunewald TG, Damke L, Maschan M, Petrova U, Surianinova O, et al. (2010) First report of effective and feasible treatment of multifocal lymphangiomatosis (Gorham-Stout) with bevacizumab in a child. Ann Oncol 8: 1733-1734.
- Ozeki M, Nozawa A, Yasue S, Endo S, Asada R, et al. (2019) The impact of sirolimus therapy on lesion size,clinical symptoms, and quality of life of patients with lymphatic anomalies. Orphanet J Rare Dis 14: 141.
- Ferrara N (2004) Vascular endothelial growth factor: basic science and clinical progress. Endocr Rev 25: 581-611.
- Cursiefen C, Chen L, Borges LP, Jackson D, Cao J, et al. (2020) VEGF-A stimulates lymphangiogenesis and hemangiogenesis in inflammatory neovascularization via macrophage recruitment. J Clin Invest 113: 1040-1050.
- Garcia J, Hurwitz HI, Sandler AB, Miles D, Coleman RL, et al. (2020) Bevacizumab (Avastin̨̉) in cancer treatment: A review of 15 years of clinical experience and future outlook. Cancer Treat Rev 86: 1020.
- Alitalo K, Tammela T, Petrova TV (2005) Lymphangiogenesis in development and human disease. Nature 438: 946-953.
- Trenor CC 3rd, Chaudry G (2014) Complex lymphatic anomalies. Semin Pediatr Surg 23: 186-190.
- Wassef M, Blei F, Adams D, Alomari A, Baselga E, et al. (2015) ISSVA Board and Scientific Committee: Vascular anomalies classification: recommendations from the International Society for the Study of Vascular Anomalies. Pediatrics 136: 203-214.
- Kransdorf MJ (1994) Benign soft tissue tumors in a large referral population: distribution of specific diagnoses by age, sex, and location. AJR Am J Roentgenol 164: 395-402.
- Braamskamp MJ, Dolman KM, Tabbers MM (2010) Clinical practice. Protein-losing enteropathy in children. Eur J Pediatr 169: 1179-1185.
- Takemura T, Watanabe M, Takagi K, Tanaka S, Aida S, et al. (1995) Thoracoscopic resection of a solitary pulmonary lymphangioma: report of a case. Surg Today 25: 651-653.
- Bermejo Casero EJ, Mongil Poce R, Arrabal SÃÆánchez R, FernÃÆández de Rota Avecilla A, BenÃÆÃÂtez DomÃÆénech A, et al. (2004) Diffuse thoracic lymphangiomatosis: diagnosis and treatment. Arch Bronconeumol 40: 599-601.
- Molitch HI, Unger EC, Witte CL, van Sonnenberg E (1995) Percutaneous sclerotherapy of lymphangiomas. Radiology 194: 343-347.
- Kandil A, Rostom AY, Mourad WA, Khafaga Y, Gershuny A, et al. (1997) Successful control of extensive thoracic lymphangiomatosis by irradiation. Clin Oncol (R Coll Radiol) 9: 407-411.
- Laforgia N, Schettini F, De Mattia D, Martinelli D, Ladisa G, et al. (2016) Lymphatic malformation in newborns as the first sign of diffuse lymphangiomatosis: successful treatment with sirolimus. Neonatology 109: 52-55.
- Wang Z, Li K, Yao W, Dong K , Xiao X, et al. (2015) Successful treatment of kaposiform lymphangiomatosis with sirolimus. Pediatr Blood Cancer 62: 1291-1293.
- Bassi A, Syed S (2014) Multifocal infiltrative lymphangiomatosis in a child and successful treatment with sirolimus. Mayo Clin Proc 89: e129.
- Kinnier CV, Eu JPC, Davis RD, Howell D N, Sheets J, et al. (2008) Successful bilateral lung transplantation for lymphangiomatosis. Am J Transplant 8: 1946-1950.
- Tammela T, Alitalo K (2010) Lymphangiogenesis: molecular mechanisms and future promise. Cell 140: 460-476.
- Dupond JL, Bermont L, Runge M, De Billy M (2010) Plasma VEGF determination in disseminated lymphangiomatosis-Gorham-Stout syndrome: A marker of activity? A case report with a 5-year follow-up. Bone 46: 873-876.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences