Congenital Bilateral Choanal Atresia: A Rare Case
Manish Gupta and Chandpreet Kour
DOI10.21767/2380-7245.100162
Manish Gupta* and Chandpreet Kour
Department of ENT, Maharishi Markandeshwar Institute of Medical Sciences and Research, Ambala, India
- *Corresponding Author:
- Manish Gupta
Professor, Department of ENT
Maharishi Markandeshwar Institute of Medical Sciences and Research
Ambala, India
Tel: 09915025819
E-mail: manishgupta1217@gmail.com
Received Date: May 23, 2017; Accepted Date: July 31, 2017; Published Date: August 03, 2017
Citation: Gupta M, Kour C (2017) Congenital Bilateral Choanal Atresia: A Rare Case. J Rare Disord Diagn Ther. 3:9. doi: 10.21767/2380-7245.100162
Abstract
Congenital Choanal Atresia (CCA) is the developmental misstep or inadequacy of the nasal cavity to connect posteriorly with the nasopharynx. Bilateral atresia presents with life threatening asphyxia at birth, while unilateral variety often remains unnoticed and presents later. This is to highlight the importance of taking into account the bilateral form in differential diagnosis of severe respiratory distress in the newborn.
In our case a full term, newborn baby presented with attacks of cyanosis and respiratory distress soon after birth. The insertion of nasal suction catheters in both nasal cavity and its non-passage into oropharynx, confirmed the diagnosis of bilateral Choanal atresia. As surgical repair is recommended at the earliest in bilateral cases thus immediate transnasal endoscopic repair was done relieving the life threatening nasal obstruction.
Keywords
Choanal atresia; Endoscopic transnasal approach; Children; Diagnosis; Management
Introduction
Congenital Choanal Atresia (CCA) is an uncommon anomaly that causes upper airway obstruction in newborns, with a frequency of 1 in 7000 to 8000 births [1]. It affects females twice more commonly than males and is frequently unilateral and right-sided than bilateral [2]. It is hypothesized to be the consequence of an abnormality of rupture of the buccopharyngeal membrane. The atresia may be classified as bony, mixed bony and membranous or purely membranous. Nature of the obstructing atretic plate has often been described as 90% bony and 10% membranous [3]. Most cases of CA are isolated malformations, but it may be associated with charge syndrome (includes coloboma, heart defect, CA, retardation of growth, genital anomalies, and ear anomalies like hypoplasia of the external ear and hearing loss) [1]. Bilateral CCA is an emergency, because immediate maintaining an airway and relieving the obstruction is essential, to avoid cyanosis and subsequent death [3]. The urgent treatment of neonates presenting with intermittent cyanosis is the insertion of an oral airway and feeding via an oro-gastric tube. The surgery gives the definitive treatment and commonly used methods are the trans-palatal approach [3], the trans-septal approach [4] and the endoscopic transnasal approach [5].
We discuss here the various diagnostic clinical and radiological methods to be followed in a rare case of bilateral CCA. Also being discussed are the various surgical modalities, with special emphasis on transnasal endoscopic approach and postoperative stenting.
Case Report
The 2.8 kg term female was born to Gravida 1, Para 1 mother via emergency caesarean, done for non progression of labour. The mother and father were 26 and 30 years old, respectively and there was no antenatal history of smoking, drugs intake, infections or exposure to teratogens. The APGAR (Appearance, Pulse, Grimace, Activity and Respiration) score at birth was 8 and 9 at 1st and 5th minute respectively. Immediately after birth she developed respiratory distress and cyanosis. On pulse oxymetry her PaO2 was 88% at room air. She was shifted to Neonatal Intensive Care Unit (NICU) for further evaluation and management. The examination in the NICU, revealed an active vigorous baby with intermittent cyanosis which resolved on crying. The respiratory rate was 50 breaths/min and required 30% FiO2 with mouth airway and face mask to maintain oxygen saturation up to 95%. The cardiac and other systemic examination was normal. Supportive treatment was started which included oxygen, intravenous fluids and prophylactic broad spectrum antibiotics. The chest X- ray was normal. Besides complete blood count, C-reactive protein and blood culture were done to rule out sepsis.
The differential diagnosis of sepsis, cyanotic congenital cardiac disease and transient tachypnea of new-born, encephalocele, tumors, dermoid or nasopharyngeal bursa was considered. The presence of intermittent cyanosis (aggravated with feeds and resolved on crying) concomitant with an unremarkable respiratory and cardiovascular examination prompted us to exclude the possibility of Choanal atresia.
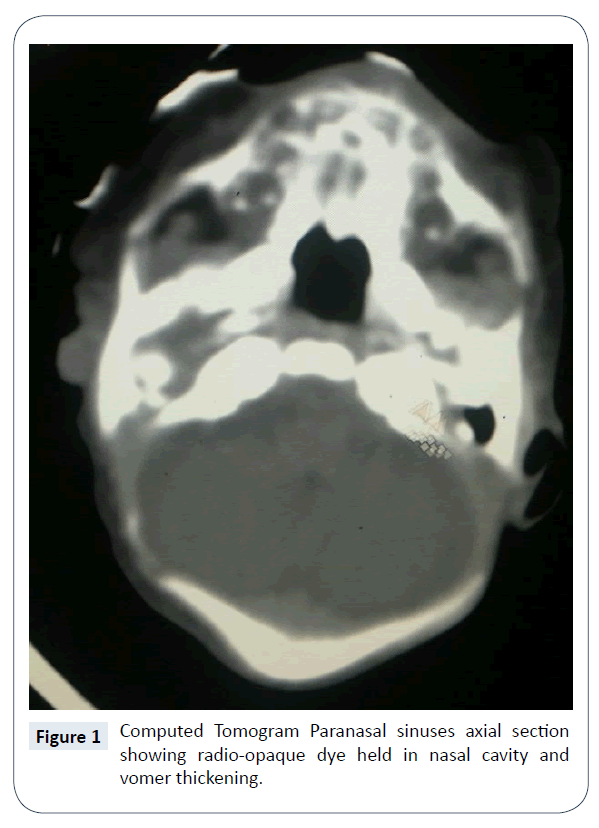
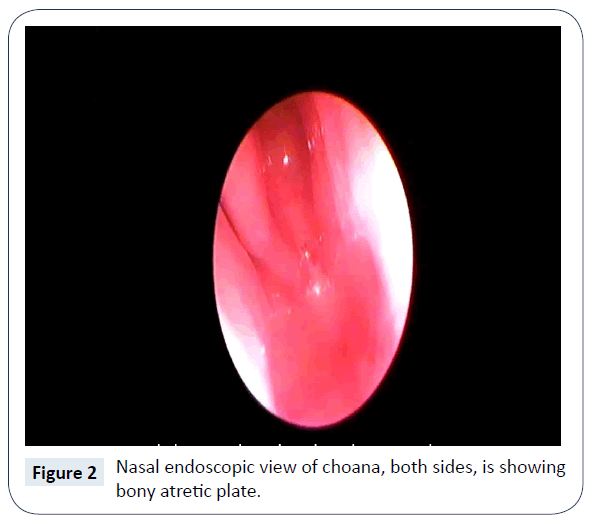
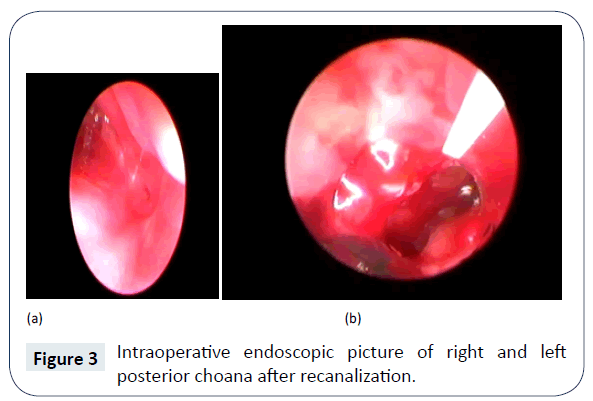
The diagnosis of bilateral Choanal atresia was established clinically by failure to pass size 5 French suction tube from nostril, nasal cavity to the pharynx. Computed Tomogram (CT) nose and paranasal sinuses confirmed the existence of bilateral, complete, bony Choanal atresia (Figure 1). There were no other associated congenital anomalies. It was further confirmed by nasal endoscopy (Figures 2 and 3) and it was planned for surgical repair/recanalization at the earliest. Still in NICU feeding was started via orogastric tube.
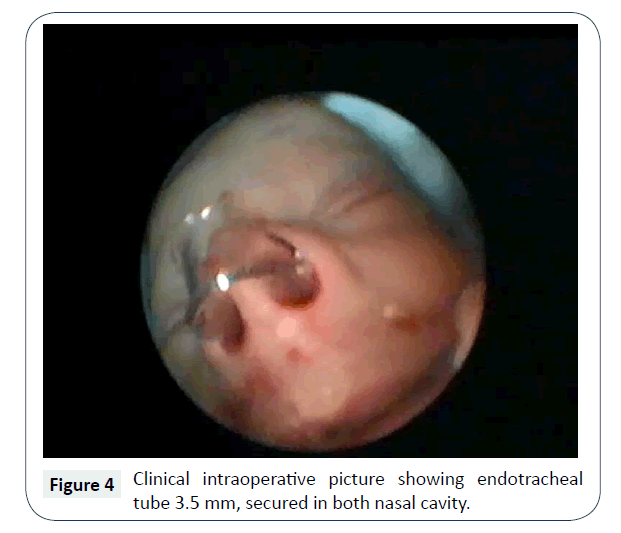
On 4th day of life patient was taken up for surgical repair via nasal route, with endoscopes and debrider, under general anaesthesia. After decongestion and suction removal of thick mucus, suction cautery was used to remove the mucosa at choana and opening made with controlled pressure of metallic nasal suction cannula, under vision from 2.7 mm, 0° nasal endoscope. Further, opening was widened using microdebrider and posterior septectomy was done using back biting forceps. Removal of posterior septum i.e., vomer helped in making a single large rectangular common opening, rather than 2 small circular ones, which are more likely to stenose by circumferential fibrosis. Also, it helped in proceeding with surgery via binostril approach. Haemostasis achieved intraoperatively, with no need of nasal packs, after surgery endotracheal tube lumen size 3.5 mm, cut to appropriate length (posterior end of this stent crosses the posterior choana and doesn’t touch posterior wall of nasopharynx), bent and partial wall removed from middle (to achieve patency of airway and allow easy passage of suction catheter), was placed bilaterally and stay suture applied anteriorly with silk (Figure 4).
Routine intravenous antibiotic coverage besides normal saline instillation and regular suction was given. Neonate remained stable post-operatively on continuous positive airway pressure for one day and on room air subsequently (Figure 5). With no intraoperative or postoperative complications documented, the patient was discharged on 4th post-operative day. She was on breast feeding at the time of discharge with no respiratory difficulty. The nasal stent was removed 4 weeks postoperatively. The child is under follow up for a year with no complaints of recurrence of symptoms or any complications.
Discussion
CCA is a developmental disorder of upper airway where no connection exists between the nasal cavity and the oropharynx. It was first described by Roderer in 1755 [1]. It is a rare congenital disorder occurring approximately one in 7000 live births [3,4]. Male to female ratio of CCA occurrence is (1:2) and unilateral atresia is more common than bilateral. CCA itself may be classified as bony, mixed i.e., bony and membranous and purely membranous.
There are various theories, trying to explain the aetiopathogenesis of choanal atresia, but the most accepted are, either failed oronasal membrane rupture or abnormal migration of neural crest cells into the nasal vault [5,6]. Though some cases are familial suggesting monogenic inheritance, the majority are sporadic [7].
Bilateral CCA causes complete nasal obstruction, leading to immediate respiratory distress and impending death due to asphyxia and cardiopulmonary arrest. This is because newborns are obligate nose breathers or instinctively breathes only through the nose until approximately 4-6 weeks at which time mouth breathing is learned. This aversion to mouth breathing has been attributed to an evolutionary need for air currents to pass over the olfactory area [8]. It has been demonstrated that the relatively higher position of the cervical viscera during infancy impedes access of air from the mouth to the lower airway, thus leaving nose only for respiration [9]. This may play a protective role against the aspiration of food in the newborn.
The typical clinical picture is cyclic cyanosis i.e., blue spells and respiratory difficulty that worsens during feeding or when child falls asleep with mouth closure. This respiratory difficulty is relieved on crying, as the mouth opens. Still, it requires high level of suspicion, to consider bilateral CCA as the differential, due to its rarity. The diagnosis in our case was confirmed when the nasogastric tube (number 5 French) failed to pass through both the nares down to oropharynx. In addition, observing misting on a metal spatula or the movement of a wisp of cotton wool placed beneath the nose are other bed side methods used for the diagnosis of choanal atresia [10]. A drop of methylene blue placed in nasal cavity, if appears in oropharynx, excludes atresia [10].
Though most cases of CCA are isolated, but the association with other congenital anomalies is known. Thus, a comprehensive general physical examination is a must, to identify other congenital anomalies. It is also essential to assess the nasal anatomy and amount of deformity by nasal and nasopharyngeal examination, using flexible or rigid fibreoptic endoscopes. Choanography (instillation of radiopaque contrast material in nares with patient in supine position) has been the traditional method of confirming the diagnosis of atresia; the modern investigation of choice, however, is computerized tomography [11]. The location, type and thickness of atresia confirmed on computed tomographic scan axial section, helps the operating surgeon in establishing a treatment plan for repair and deal with associated abnormalities, like high arched hard palate, thickened vomer, septum and lateral nasal structures, which further reduce the diameter of nasal fossa and the nasopharynx [10].
McGovern had described the use of a large holed rubber nipple, which when strapped in the infant’s mouth, acts as oropharyngeal airway for temporary relief [12]. Endotracheal intubation is usually not required until the patient needs mechanical ventilation. The surgical recanalization is the mainstay of treatment. Out of all the various approaches for opening the posterior choana, the transseptal, transpalatal and the endoscopic transnasal approaches are more commonly followed. There are various factors which decide which particular approach is useful in which patient. They are, age of the patient, size of nasopharynx, thickness of the atresia, bony vs membranous, bilateral vs. unilateral and the need of post-operative stenting. The transpalatal approach is preferred in unilateral choanal atresia, but results in abnormal palatal growth, palatal fistula and further orthodontic problems, like cross bite [10]. The transseptal approach is impractical in infants. The endoscopic transnasal approach is considered better due to simplicity with minimal invasion and blood loss, excellent visualization, access and high rate of success, with less recovery period and less morbidity [13]. Availability of rigid thin endoscopes with powerful light source and High definition camera has improved the transnasal technique and studies continue to demonstrate increasing support for this [14,15]. Transnasal puncture of CA and dilatation, followed by stenting with endotracheal portex tubes for 3-4 weeks is the surgical procedure of choice [16]. Better results, with less chance of re-stenosis have been reported with application of topical mitomycin C intraoperatively [17].
With use of stents to maintain patency, various complications had been described, which include local infection, foreign body reaction, formation of granuloma and nasal synechia [18]. They may contribute to choanal restonsis. None such complication occurred in our case.
Conclusion
Bilateral CCA is a rare disorder and is medical, surgical emergency. It should be suspected in newborn with a history of cyclical cyanosis and is diagnosed by failure to insert 6-F nasal catheters through the nares into the nasopharynx. CT scan of the nasal cavity and nasopharynx not only confirms the diagnosis but also defines the extent and type of atresia and helps in deciding the surgical approach. The endoscopic transnasal approach for opening the choana is preferred now days due to better access, higher success rate and less morbidity.
References
- Leclerc JE, Fearon B (1987) Choanal atresia and associated anomalies. Int J Pediatr Otorhinolaryngol 13: 265-272.
- Sadek SAA (1998) Congenital bilateral choanal atresia. Int J Pediatr Otorhinolaryngol 42: 247-256.
- Azar RH, Younis RT (1995) Transnasal repair of choanal atresia using telescopes. Arch Otolaryngol Head Neck Surg 121: 517-520.
- Samadi DS, Shah UK, Handler SD (2003) Choanal atresia: a twenty year review or medical comorbidities and surgical outcomes. Laryngoscope 113: 254-258.
- Heneger AS, Strom M (2009) Choanal atresia: A new embryonic theory and its influence on surgical management. Laryngoscope 92: 913-921.
- Dunham ME, Miller RP (1992) Bilateral choanal atresia associated with malformation of the anterior skull base: embryogenesis and clinical considerations. Ann Otol Rhinol Laryngol 101: 916-919.
- Harris J, Robert E, Kallen B (1997) Epidemiology of choanal atresia with special refence to the CHARGE association. Pediatrics 99: 363-367.
- Williams HJ (1971) Posterior choanal atresia. The American J of Roentgenology 112: 1-11.
- Moss ML (1965) Veloeiglottic sphincter and obligate nose breathing in neonate. J Pediat 67: 330-331.
- Assanasen P, Metheetrairut C (2009) Choanal Atresia. J Med Assoc Thai 92: 699-706.
- Myer CM (1983) Cotton RT. Nasal obstruction in the pediatric patient. Pediatrics 72: 766-777.
- McGovern FH (1953) Association of congenital choanal atresia and congenital heart disease: report of two cases. Ann Otol Rhin & Laryng 62: 894-895.
- Hathiram BT, Grewal DS (2000) Endoscopic endonasal emergency management of bilateral choanal atresia in new borns. Indian J Otolaryngol Head Neck Surg 52: 102-103.
- James DR, Paolo C, Vito F (2009) Choanal atresia and choanal stenosis. Otolaryngologic Clinics of North America 42: 339-352.
- Holland BW, McGuirt WF (2001) Surgical management of choanal atresia: improved outcome using mitomycin. Arch Otolaryngol Head Neck Surg 127: 1375-1380.
- Stankiewicz JA (1999) The endoscopic repair of choanal atresia. Otolaryngol Head Neck Surg 103: 931-937.
- Kumar AMS, Naik AS, Praveen DS (2005) Choanal atresia: Experience with transnasal Endoscopic technique. Ind J Otolaryngol Head Neck Surg 57: 96-98.
- Van Den Abbeele T, Francois M, Nancy P (2002) Transnasal endoscopic treatment of choanal atresia without prolonged stenting. Arch Otolaryngol Head Neck Surg 128: 936-940.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences