Clinical Representation of Hematohidrosis: A Case Report
Shreyash Narendra Birar*, Dileep Babasaheb Kadam and Gajanan Balaji Kurundkar
Department of Internal Medicine, Maharashtra University of Health Sciences, Pune, India
Published Date: 2024-08-30DOI10.36648/2380-7245.11.4.155
Shreyash Narendra Birar*, Dileep Babasaheb Kadam and Gajanan Balaji Kurundkar
Department of Internal Medicine, Maharashtra University of Health Sciences, Pune, India
- *Corresponding Author:
- Shreyash Narendra Birar
Department of Internal Medicine, Maharashtra University of Health Sciences, Pune,
India,
Tel: + 91-9423128146;
E-mail: shreyash.birar@gmail.com
Received date: August 11, 2024, Manuscript No. IPRDDT-24-19519; Editor assigned date: August 13, 2024, PreQC No. IPRDDT-24-19519 (PQ); Reviewed date: August 19, 2024, QC No. IPRDDT-24-19519; Revised date: August 23, 2024, Manuscript No. IPRDDT-24-19519 (R); Published date: August 30, 2024, DOI: 10.36648/2380-7245.11.4.155
Citation: Birar SN, Kadam DB, Kurundkar GB (2024) Clinical Representation of Hematohidrosis: A Case Report. J Rare Disord Diagn Ther Vol.11 No. 4:155.
Abstract
Hematohidrosis is indeed a rare and intriguing condition. It's thought to occur when the tiny blood vessels around the sweat glands rupture, leading to blood mixing with sweat. This phenomenon is often linked to severe stress or emotional trauma, though the precise pathophysiological mechanisms remain unclear. Diagnosing hematohidrosis involves ruling out other possible causes of blood in sweat such as bleeding disorders, vasculitis, or other dermatological conditions. Treatment typically focuses on addressing the underlying stressors, emotional factors and ensuring that any contributing medical conditions are managed.
Here, we present a case of hematohidrosis in a 17 year old male who had bleeding from several sites like forehead, face, scalp, eyes, nose and ears around six to seven times per day in the last 2 months. During hospitalization, the patient was thoroughly investigated but no clear cut etiology could be pointed out. Patient underwent skin biopsy and was diagnosed with hematohidrosis and treated with beta blockers and antidepressants. His condition had improved significantly on follow-up.
Keywords
Hematohidrosis; Antidepressants; Beta blockers; Bleeding time; Anti-cholinergic drugs; Headache
Introduction
Hematohidrosis is a sweat gland disorder characterized by blood in sweat [1]. Patients bleeds from the skin and mucous membranes of face, forehead, palms, ear and other sites which is not related to a skin injury or trauma. Very few number of cases have been reported till date. Asia and Africa account for the majority epidemiological distribution [2].
Stress and Anxiety is considered as the biggest contributor in majority cases. In summary, while hematohidrosis is often associated with stress or trauma, idiopathic cases where no clear cause is identified remain a significant area of interest in medical research. Understanding these cases better could provide valuable insights into the condition’s underlying mechanisms and improve diagnostic and therapeutic approaches [2].
To diagnose hematohidrosis, several key criteria must be fulfilled:
Verified recurrent spontaneous and self-Limiting blood discharge: This must be observed and documented by healthcare professionals, ensuring that the bleeding is not caused by external injuries or self-inflicted wounds.
Microscopic examination: Analysis of the secretions should reveal the presence of various blood components, confirming that the discharge contains blood.
Intact area of bleeding: The area from which the blood is released should be undamaged, without any signs of abrasions or external injuries, indicating that the bleeding originates from within the sweat glands or skin. Additionally the benzidine test serves as a laboratory method to confirm the presence of blood in the sweat. This test works as follows:
Haemoglobin reaction: Haemoglobin in the blood reacts with hydrogen peroxide.
Colour development: This reaction produces oxygen and compounds that produce a colour change, typically ranging from green to blue, indicating the presence of blood. These diagnostic procedures help to accurately identify hematohidrosis and distinguish it from other conditions with similar symptoms.
Case Presentation
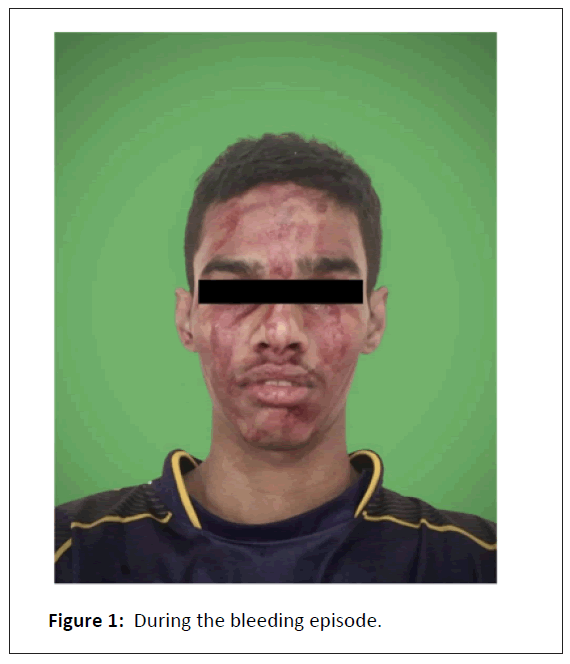
17 year old male with no known comorbidities presented to medicine OPD (Out Patient Department) with chief complaints of oozing of blood from his scalp, forehead, face, ears and nose around six to seven times a day for the last 2 months. Such episodes lasted for around 20 to 30 minutes. They were preceded by a throbbing type of headache for 5 to 10 minutes followed by tingling sensation over the scalp and face and then by oozing of blood from the same sites (Figure 1).
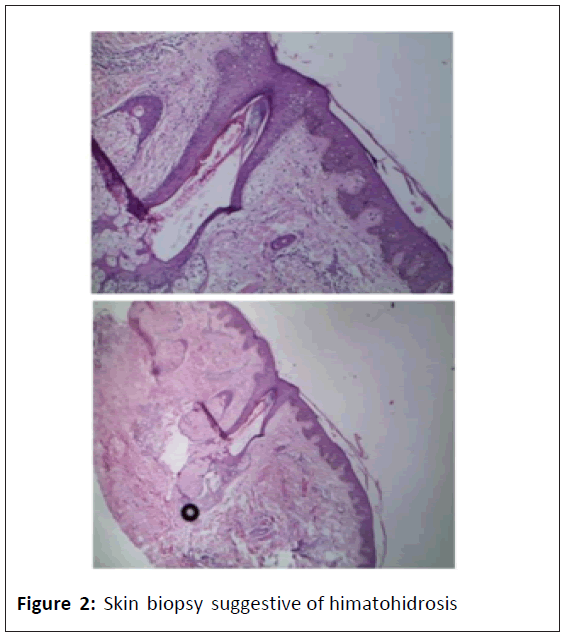
Patient was alright during the post exposure period till the next episode. No bruising, cuts, abrasions and telangiectasia. No local tenderness. There was no history of any bleeding from other sites. No history of ingestion of any antiplatelets or anticoagulants. No such episodes were noted in the past or in the family. Such episodes started 2 months back post stress due to family separation and his mother’s deteriorating health. On physical examination, the patient was anxious. His systemic examinations did not reveal any abnormality. Routine investigations including complete blood count, bleeding time, clotting time, active partial thrombin time, prothrombin time and INR, (International Normalized Ratio) liver function tests and renal function tests were within normal limits. Urine and stool examination did not reveal any red blood cells. Upper gastrointestinal endoscopy and ultrasound of the abdomen did not reveal any abnormality. Skin biopsy was taken from the forehead and histopathological findings showed numerous dilated capillaries in superficial papillary dermis surrounded by lymphocytic in filtrations and extravasation of red blood cells suggestive of hematohidrosis. Psychiatry evaluation was suggestive of generalised anxiety disorder and clinical depression. Frequency and severity of subsequent episodes decreased with benzodiazepines, anti-depressants, beta-blockers and anticholinergic drugs. Patient is still under follow up (Figure 2).
Histopathology of skin biopsy shows numerous dilated capillaries in superficial papillary dermis which are surrounded by mild lymphocytic infiltrate. Additionally, there is extravasation of RBC’s and hemosiderin noted in papillary dermis deep dermis shows eccrine glands which are intermingled with small capillaries containing RBC’s. The capillaries are also associated with straight portions of eccrine duct in the mid dermis as well as close to the follicle. Overlying epidermis and stratum corneum is normal.
Results and Discussion
Hematohidrosis is a rare condition characterized by the presence of blood in sweat. It can occur in individuals experiencing extreme levels of stress [3]. The blood seeps into the sweat ducts due to vasculopathies in the dermal vasculature and increased sympathetic activation from acute stress and anxiety. This leads to peri-glandular vascular constriction followed by subsequent dilation [4,5]. Numerous blood vessels, arranged in a net-like structure around the sweat glands, contract and then expand to the point of rupture under significant stress. As a result, blood flows into the sweat glands, which are pushed to the surface, manifesting as droplets of blood mixed with sweat [5,6]. This mechanism helps explain why individuals with anxiety, high blood pressure, or elevated sympathetic nervous system tone experience hematohidrosis more frequently.
According to a systematic review done in 2023, there are 74 articles with 106 hematidrosis cases. 40 from India and 11 from China report the majority of cases. Patients are mostly females having 76.5% predisposition with a median age of 13 years. Most common bleeding site is the head region. Headaches (26.9%) and abdominal pain (16.4%) are the most frequently reported prodromal symptoms. Beta-blockers (43%) and anxiolytics (23.2%) are the most commonly prescribed medications. Psychotherapy (37.5%) and counselling (32.5%) are the most frequently used non-pharmacological treatments. Only 41.1% of cases achieve complete resolution, and just 19.8% of cases are highly likely to be hematohidrosis [7].
Conclusion
It is vital to raise awareness about hematohidrosis given its frightening nature and potential for unnecessary testing. Educating physicians globally can help in understanding this rare yet alarming condition, leading to better management and outcomes for patients. Early detection, even in the absence of underlying diseases or psychological stressors, is key for successful treatment and achieving complete remission.
Updating the registry of this disease is indeed vital for collecting comprehensive data. A well-maintained registry helps ensure a sufficient sample size, which is essential for conducting robust epidemiological and clinical studies. This can significantly enhance our understanding of the disease's pathophysiology, improve diagnostic and treatment strategies, and ultimately contribute to better patient outcomes. The data collected can also help identify trends, risk factors and potential areas for further research.
References
- Tshifularo M (2014) Blood otorrhea: Blood-stained sweaty ear discharges: Hematohidrosis; four case series (2001–2013). Am J Otolaryngol 35: 271-273.
[Crossref] [Google scholar] [Indexed]
- Kluger N (2018) Hematidrosis (bloody sweat): A review of the recent literature (1996-2016). Acta Dermatovenerol Alp Pannonica Adriat 27: 85-90.
[Crossref] [Google scholar] [Indexed]
- Panconesi E, Hautmann G (1999) The spectrum of plasminogen activator-dependent fibrinolysis-altered psychoinduced vasopermeability syndrome. Clin Dermatol 17: 609-613.
[Crossref] [Google scholar] [Indexed]
- Jafar A, Ahmad A (2016) Child who presented with facial hematohidrosis compared with published cases. Case Rep Dermatol Med 2016: 5095781.
[Crossref] [Google scholar] [Indexed]
- Gilbert GSO, Koleta T, Garniasih D, Yanto TA (2021) Hematidrosis and hemolacria: Report of two cases from indonesia. Ir J Blood and Ca. 13: 98-101.
- Uber M, Robl R, Abagge KT, Carvalho VO, Ehlke PP et al. (2015) Hematohidrosis: Insights in the pathophysiology. Int J Dermatol Dec 54: 542-543.
[Crossref] [Google scholar] [Indexed]
- Octavius GS, Meliani F, Heriyanto RS, Yanto TA (2023) Systematic review of hematidrosis: Time for clinicians to recognize this entity. World J Dermatol 11: 7-29.
[Crossref]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences