A Pre-operative Realignment of Atlanto-occipital Dislocation
Wilson J, Ginsberg J, Paullus CP and Santos PA
DOI10.21767/2380-7245.100168
Wilson J, Ginsberg J, Paullus CP and Santos PA*
Department of Surgery, Penn State Health Milton S. Hershey Medical Center, Hershey, Pennsylvania, USA
- *Corresponding Author:
- Ariel P Santos
Department of Surgery
Texas Tech University Health Science Center
Lubbock, Texas
Tel: +1717-531-0003
E-mail: ariel.santos@ttuhsc.edu
Received Date: August 05, 2017; Accepted Date: September 19, 2017; Published Date: September 25, 2017;/p>
Citation: Santos PA, Wilson J, Paullus CP (2017) A Pre-operative Realignment of Atlanto-occipital Dislocation. J Rare Disord Diagn Ther 3:15. doi: 10.21767/2380-7245.100168
Abstract
Atlanto-occipital dislocation (AOD) is the most common cervical spine injury in motor vehicular accident fatalities. It carries a high morbidity and mortality. Diagnosis of this injury is difficult and requires a high index of clinical suspicion combined with careful examination of imaging modalities. A 22-year-old female was in a motor vehicle accident and was found unresponsive. She sustained multiple injuries requiring emergency laparotomy and damage control laparotomy. CT of Cervical spine was initially read as negative. Ten days later, the patient had no movement of her lower extremities. It was discovered that craniocervical dissociation was missed on the CT done on admission; CT angiogram done to rule out blunt carotid and vertebral artery injury showed realignment of the spine. The patient underwent surgery and recovered the use of her legs. Spontaneous realignment pre-operatively for AOD has not been reported in the literature because most cases underwent immediate surgery for stabilization.
Keywords
Spine injury; CT; Magnetic resonance imaging; Surgery
Introduction
Atlanto-occipital dislocation (AOD) is a devastating and highly unstable cranio-cervical injury caused by high impact trauma, usually in the form of a motor vehicle accident (MVA). AOD accounts for 6-8% of all motor vehicle accident fatalities and is the most common cervical spine injury in motor vehicle accident fatalities [1]. It is often associated with high morbidity and mortality. This often-fatal injury has increased survival with improved pre-hospital care, immediate inline cervical stabilization, prompt diagnosis, and proper treatment.
The occipito-atlantal joint consists of bony articulations supported by ligaments. The occipital condyles articulate with the lateral masses of C1. Ligaments such as the tectorial membrane, alar ligaments, Barkow ligament, and the cruciate ligament all play a role in structural support [1]. The tectorial ligament limits excessive flexion and extension. The alar ligament limits contralateral flexion and axial rotation. The Barkow ligament prevents neck extension. The cruciate ligament limits lateral motion of C1 relative to the dens [1]. A disruption of these ligaments leads to craniocervical instability and puts the patient at a tremendous risk for spinal cord injury. The diagnosis of AOD is challenging to determine on plain film x-ray due to difficulty identifying landmarks, and often requires the use of a cervical CT. High clinical suspicion is needed to properly diagnose this injury promptly in order to improve patient outcomes. Proper management can sometimes have complicated by presentation. Neurogenic shock may be the presenting symptom which can delay diagnosis and treatment. AOD is treated with surgical fixation; however, this case demonstrates realignment in a patient before intervention.
Case Presentation
The patient is a 22-year-old restrained, female driver who was involved in a MVA. Patient was noted to be unresponsive and was endotracheally intubated with inline cervical stabilization and maintained on cervical collar. She was resuscitated with crystalloids and was given two units of pRBC blood. With the hypotension and positive FAST examination, she was taken for an emergency laparotomy, perihepatic packing with subsequent closure and removal of packing the next day. The patient had bilateral pulmonary contusions with right pneumothorax requiring chest tube thoracostomy, bladder contusion, closed fracture of right transverse processes (L1, L2, L5), liver laceration, pubic ramus fracture, and a closed displaced fracture of multiple ribs on the right. She presented with an injury severity score (ISS) of 38. Ten days after the MVA, the patient was awake, and she was tracking and following commands with her eyes. She was withdrawing to pain with the upper extremities; however, she had no movement of her lower extremities. When neurosurgery was consulted, they found a craniocervical dissociation that was missed on a cervical CT done on admission. However, a CT angiogram done ten days after the accident showed realignment of the spine. Magnetic resonance imaging (MRI) of the cervical spine showed findings consistent with cranio-cervical dissociation with rupture of tectal membrane and alar ligaments. Eleven days status post MVA, the patient underwent an occipital plate placement with par screws at C2, lateral mass screws C3, C4, and C5 for definitive stabilization of the cranio-vertebral junction. She required tracheostomy and percutaneous endoscopic gastrostomy tube placement on post injury day 16. She was eventually weaned off the ventilator. Patient underwent early physiotherapy and worked with speech language pathologist. Her PEG tube was removed and Tracheostomy tube decannulated. She was able to move all extremities on command 45 days after the accident. The patient had a hospital stay of three and a half months and she was able to walk with assistance on discharge.
Discussion
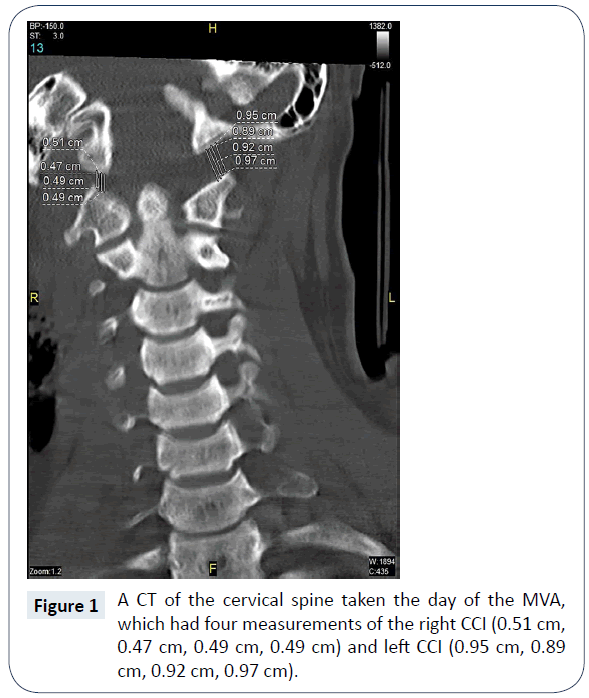
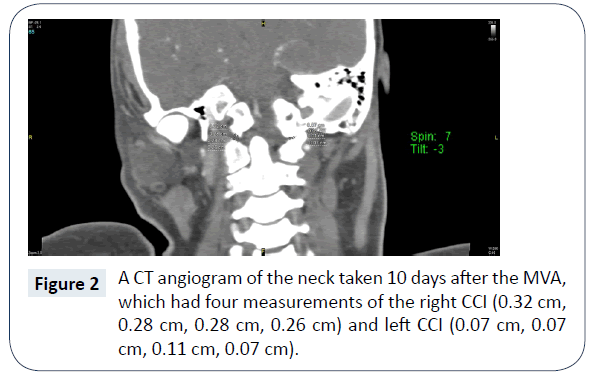
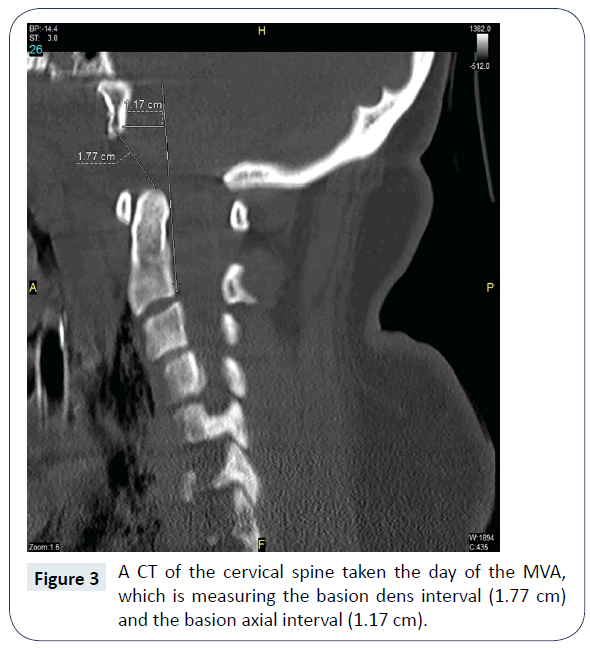
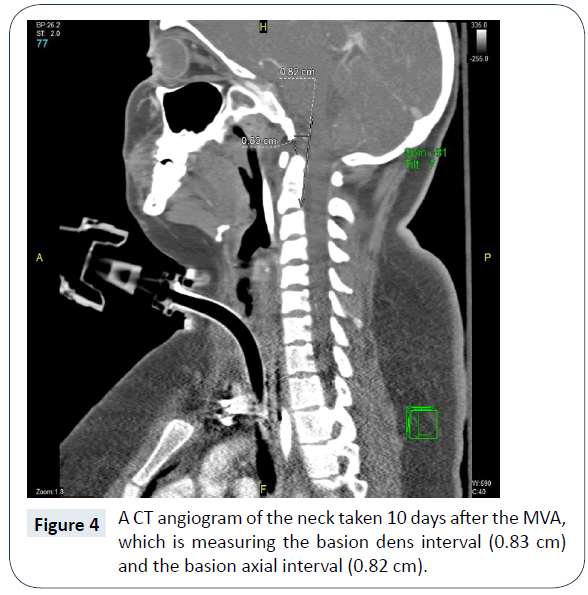
AOD is often difficult to diagnose and requires the use of imaging for a proper diagnosis. New data has shown that the most sensitive test for this diagnosis is a CT-based occipital condyle-C1 interval (CCI) [1]. The basion dens interval (BDI) measures the distance between the basion and dens, and it is positive for AOD when the BDI >12 mm [1]. On the original CT, the patient had a positive CCI and BDI test, indicating a diagnosis of AOD.
A study has shown that a diagnosis of AOD is more likely to be missed on initial CT of patients with a high ISS [2]. The patient presented with an ISS score of 38 and came in with a remarkable amount of injuries. This further illustrates the importance of having a high clinical suspicion for this type of injury when patients come into the hospital from a high-energy trauma [1].
The AOD had realigned and improved in a matter of ten days without surgery. The coronal CCI on initial trauma was 4.9 mm on the right and 9.3 mm on the left (Figure 1). Ten days later the coronal CCI was 2.8 mm on the right and 0.8 mm on the left (Figure 2). The BDI was 17.7 mm (Figure 3) compared to 8.3 mm ten days later (Figure 4). Ligamentotaxis is a possible mechanism for this realignment through distraction forces transferred through intact ligaments resulting in an indirect decompression of the spinal cord [3]. In the thoracolumbar spine, ligamentotaxis aligns bony articulations mainly through the posterior longitudinal ligament, which becomes the tectorial membrane at C2 [4]. While this is an unusual case, an argument could be made to conduct animal studies in a biomechanical laboratory to determine the role each ligament plays in ligamentotaxis and if AOD realignment can be consistently reproduced in a controlled setting.
Even with realignment, surgical fixation was pursued. Early aggressive surgical stabilization is associated with improved outcomes after AOD and conservative treatment with external immobilization demonstrated a 30% rate of continued cranio-cervical instability and neurological worsening on follow-up [5].
Learning points
• Diagnosis of AOD is easy to miss and it requires a high index of suspicion and careful analysis of imaging modalities.
• Imaging should always correlate with the clinical findings, if not even in setting of normal readings the CT needs to be reviewed or MRI requested.
• AOD injuries can potentially realign without surgical intervention.
• Once identified, prompt treatment of AOD results in a more favorable patient outcome.
References
- Hall GC, Kinsman MJ, Nazar RG, Hruska RT, Mansfield KJ, et al. (2015) Atlanto-occipital dislocation. World J Orthop 6: 236-243.
- Mendenhall SK, Sivaganesan A, Mistry A, Sivasubramaniam P, McGirt MJ, et al. (2015) Traumatic atlantooccipital dislocation: comprehensive assessment of mortality, neurologic improvement, and patient-reported outcomes at a Level 1 trauma center over 15 years. Spine J 15: 2385-2395.
- Whang PG, Vaccaro AR (2007) Thoracolumbar fracture: posterior instrumentation using distraction and ligamentotaxis reduction. J Am Acad Orthop Surg 15: 695-701.
- Kuner EH, Kuner A, Schlickewei W, Mullaji AB (1994) Ligamentotaxis with an internal spinal fixator for thoracolumbar fractures. J Bone Joint Surg Br 76: 107-112.
- Diagnosis and management of traumatic atlanto-occipital dislocation injuries. Neurosurgery 50: S105-S113.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences