Obstructive Sleep Apnea Syndrome Associated with Soft Palate Pleomorphic Adenoma: Case Report and Review of Literature
Jelena Todic, Yves Jaquet and Michel-André Hotz
DOI10.21767/2380-7245.100185
Jelena Todic*, Yves Jaquet and Michel-André Hotz
Department of Otorhinolaryngology, Head and Neck Surgery, Hôpital de Pourtalès, Neuchâtel, Switzerland
- *Corresponding Author:
- Jelena Todic
Department of Otorhinolaryngology
Head and Neck Surgery, Hôpital de Pourtalès
Neuchâtel, Switzerland
Tel: +41327133000
E-mail: jelena.todic@hotmail.ch
Received Date: June 21, 2018; Accepted Date: July 12, 2018; Published Date: July 19, 2018
Citation: Todic J, Jaquet Y, Hotz MA (2018) Obstructive Sleep Apnea Syndrome Associated with Soft Palate Pleomorphic Adenoma: Case Report and Review of Literature. J Rare Disord Diagn Ther. 4:17. DOI: 10.21767/2380-7245.100185
Abstract
Context: Pleomorphic adenoma is the most common benign tumor arising in the salivary gland. Soft palatine localisation is rare but can cause an obstructive syndrome. We report a case of pleomorphic adenoma of the soft palate causing obstructive sleep apnea (OSA).
Case report: A 62-year-old woman was addressed to ENT consultation because of obstuctive sleep-disorderd breathing. On physical exam we discovered a submucosal mass of the right soft palate of 3 x 2 cm. Therapy consisted of a tumor excision. Histopathology spoke in favour of a pleomorphic adenoma. Excision of the local mass led to sleep exam normalization and symptoms resolution.
Conclusion: Oropharyngeal and oral cavity tumors may cause obstuctive sleep-disorderd breathing. All patients with sleep disordered should undergo a thorough ENT clinical examination.
Keywords
Sleep-disorderd breathing; Palatine mass; Pleomorphic adenoma
Introduction
Pleomorphic adenoma is a common salivary benign tumor mostly affecting parotid glands. It draws its name from its histological architecture which can be subdivided in three types: classical, myxoid and hypercellular. The myxoid type accounts for more than half of cases. In the major salivary glands, the tumor is enclosed by a layer of fibrous tissue termed a capsule. Incomplete capsule is observed in 33-49% of pleomorphic adenomas [1]. A small minority of tumors are located in the oral and nasal cavity [2]. They appear as slowly growing mass usually without symptoms. The differential diagnosis includes abscess, cysts, fibroma, lipoma, neurofibroma or squamous cell carcinoma [3,4]. Tumour spillage increases the risk of recurrence. Meticulous surgical excision with capsular integrity is the treatment of first choice. Recurrence is described in about 46% of cases and risk of malignant transformation in 3.3 to 13% [1]. It is rarely associated with obstructive sleep-disordered breathing. Obstructive sleep apnea (OSA) is a common well recognised entity mainly caused by obesity. The Apnea-Hypopnea Index (AHI) is defined as the number of apneas or hypopneas per hour of sleep and is mapped to disease severity [5]. Patients are considered to have OSA if their AHI is greater than 15 or if they have minimum oxygen saturation below 90 (American Academy of Sleep Medicine). In 1981, Moses et al. first reported a patient with OSA caused by nasopharyngeal carcinoma [6]. Since then 30 articles about tumors of the upper aerodigestive tract causing sleep disorder have been published [7,8]. Rada et al. studied the relationships between OSA and head and neck tumors [9]. The most frequent localisations were salivary gland, larynx, nasopharynx and oropharynx. There were 16 benign and 8 malignant neoplasms. The most frequent benign neoplasm related to OSA were lipomas. Among malignant lesions the most common were squamous cell carcinoma and non-Hodgkins lymphoma. We report a case of pleomorphic adenoma of the soft palate causing OSA and make a literature review.
Case Report
A 62-year-old woman was addressed to Ear Nose and Throat (ENT) consultation because of sleep obstructive breathing disordered symptoms including snoring and daytime fatigue.
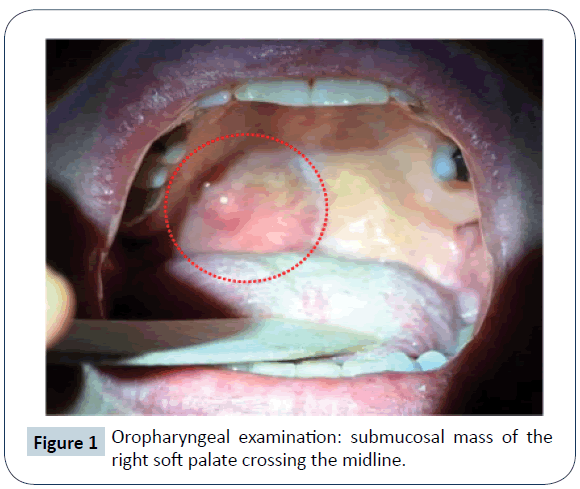
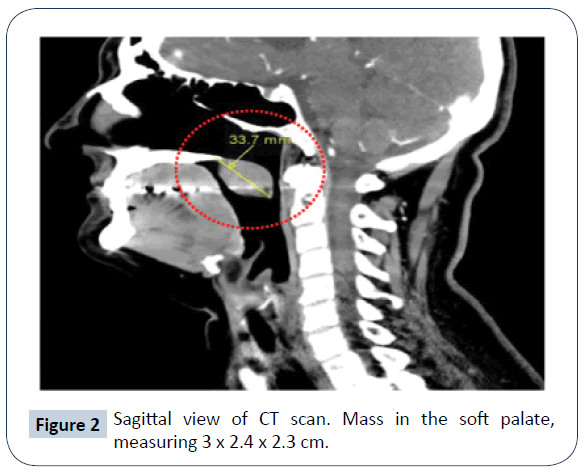
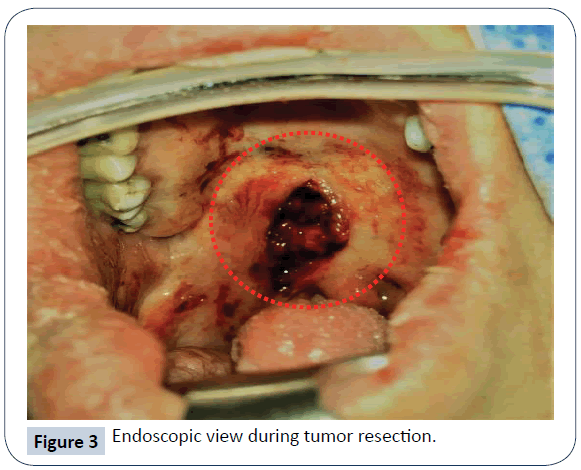
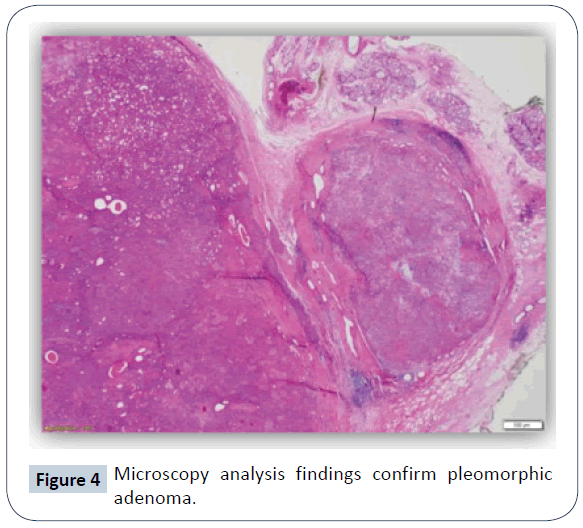
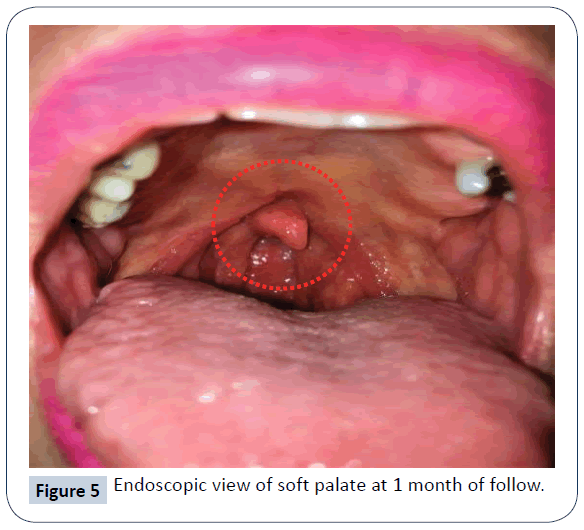
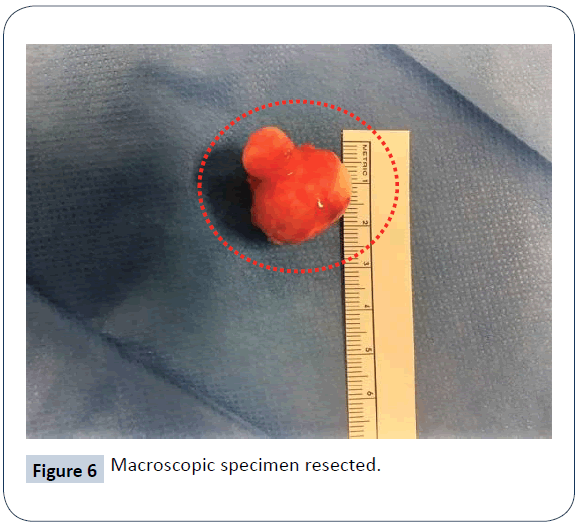
She was non-smoker and had a social alcohol consumption. The ENT work-up included clinical exam, head and neck computed tomographic scan and sleeping test. On physical exam we discovered a submucosal mass of the right soft palate crossing the midline (Figure 1). The patient had a good oral care and satisfactory dental condition. There was no mucous lesion in the oral cavity and no cervical lymph node. The rest of the ENT exam was normal. The computed tomographic scan identified a mass of 3 × 2.4 × 2.3 cm in the soft palate without invasion of the adjacent tissues (Figure 2). Preoperative polygraphy confirmed OSA with AHI of 17, 2 per hour (Table 1). Therapy consisted of surgical tumor removal preserving the soft palate (Figure 3). No OSA surgery was performed. The defect of the soft palate was treated by primary closure without reconstruction. Histopathology concluded to entirely resected pleomorphic adenoma (Figure 4). Soft palate healed without complication (Figure 5). Snoring during night disappeared. Postoperative polygraphy realised 6 months later confirmed normal sleep with AHI of 5, 9 per hour (Figure 6 and Table 1).
| Pre operative (29.11.17) |
Post opoperative (01.06.18) |
|
|---|---|---|
| IAH | 17.2 (<5/h) | 5.9 (<5/h) |
| ODI | 21.4 (<5/h) | 11.1 (<5/h) |
| Period of 02 <90% | 349 min (66%) | 50 min (15%) |
Table 1: Pre- and postoperative polygraphy, AHI=Apnea- Hypopnea Index, ODI=Oxygen Desaturation Index.
Discussion
Pleomorphic adenoma accounts for approximately 60% of all salivary gland neoplasms [10]. A small minority of tumors are located in the oral cavity, neck and nasal cavity [4,11]. In those localisations it appears as slowly growing painless mass [9] usually in the fourth or fifth decade of life, with a higher frequency in female [4,1]. The diagnosis is established on the basis of history, physical examination and histopathology [12]. Computed tomography scan and MRI can provide information on the location and size of the tumor, besides extension to surrounding structures [13,14]. Treatment consists of surgical tumor excision and/or continuous positive airway pressure [9]. Recurrence is rare after complete removal and the prognosis is excellent [15-17]. In the English-language literature, nine articles relate pleomorphic adenomas causing OSA; five cases of deep-lobe parotid tumors extending into the parapharyn-geal space [18-22], four cases arising from the minor salivary gland in the oral cavity and pharynx [23-27]. Tumors of the upper aerodigestive tract causing secondary OSA have been rarely reported in large series. Rada et al. [9] make a review finding only 30 articles about OSA caused by head-and-neck tumors, including 16 benign and 8 malignant neoplasms. Payne et al. [27] conclude that 13 of 17 (76.4%) patients with oral and oropharyngeal cancer have OSA. The most common symptom is sudden aggravation of snoring or gasping during night [17,27].
Conclusion
All patients with sleep disordered breathing should undergo a thorough ENT clinical examination [12,21]. Oral cavity and oropharyngeal tumors belong to the differential diagnosis of OSA. Sudden aggravation of snoring should raise suspicion of an oropharyngeal tumor.
References
- De Sousa Lopez ML, Amorim Barroso KM, Gomes Henriques AC, Dos Santos JN, Martins MD, et al. (2016) Pleomorphic adenomas of the salivary glands: retrospective mutlicentric study of 130 cases with emphasis on histopathological features. Eur Arch Otorhinolaryngol 274: 543-551.
- Pires FR, Pringle GA, de Almeida OP, Chen SY (2007) Intra-oral minor salivary gland tumors: a clinicopathological study of 546 cases. Oral Oncol 43: 463-470.
- Ansari MH (2007) Salivary gland tumors in an Iranian population: a retrospective study of 130 cases. J Oral Maxillofac Surg 65: 2187-2194.
- Toida M, Shimokawa K, Makita H, Kato K, Kobayashi A, et al. (2005) Intraoral minor salivary gland tumors: a clinicopathological study of 82 cases. Int J Oral Maxillofac Surg 34: 528-532.
- Young T, Peppard PE, Gottlieb DJ (2002) Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med 165: 1217-1239.
- Moses FM, Buscemi JH (1981) Obstructive sleep apnea syndrome associated with nasopharyngeal carcinoma. West J Med 134: 69-70.
- Stradling JR, Davies RJ (2004) Obstructive sleep apnoea/hypopnoea syndrome: definitions, epidemiology, and natural history. Thorax 59: 73-78.
- Koenig S (2001) Pulmonary complications of obesity. Am J Med Sci 321: 249-279.
- Rada R (2005) Obstructive sleep apnea and head and neck neoplasms. Otolaryngol Head Neck Surg 132: 794-799.
- Pinkston JA, Cole P, Incidence rates of salivary gland tumors: results from a population-based study. Otolaryngol Head Neck Surg 120: 834-840.
- Vellios F, WG Shafer (1959) Tumors of the intraoral accessory salivary glands. Surg Gynecol Obstet 108: 450-456.
- Casale M, Frari V, Vincenzi B, Bressi F, Quattrocchi CC, et al. (2012) Upper airway study should always come before any sleep study in OSAS evaluation: a giant parapharyngeal lipoma behind OSAS. Eur Rev Med Pharmacol Sci 16: 106-109.
- Bullerdiek J, Wobst G, Meyer-Bolte K, Chilla R, Haubrich J, et al. (1993) Cytogenetic subtyping of 220 salivary gland pleomorphic adenomas: correlation to occurrence, histological subtype, and in vitro cellular behavior. Cancer Genet Cytogenet 65: 27-31.
- Tuncyurek O, Eyigor H, Ozkul A (2011) What is the importance of radiology in the obstructive sleep apnea?. J Craniofac Surg 22: 1971-1973.
- Marioni G, Marino F, Stramare R, Marchese-Ragona R, Staffieri A, et al. (2003) Benign metastasizing pleomorphic adenoma of the parotid gland: a clinicopathologic puzzle. Head Neck 25: 1071-1076.
- Bradley PJ (2005) Metastasizing pleomorphic salivary adenoma should now be considered a low-grade malignancy with a lethal potential. Curr Opin Otolaryngol Head Neck Surg 13: 123-126.
- Sabesan T, Ramchandani PL, K Hussein (2007) Metastasising pleomorphic adenoma of the parotid gland. Br J Oral Maxillofac Surg 45: 65-67.
- Pang KP, Goh CHK, Tan HM (2002) Parapharyngeal space tumours: an 18 year review. J Laryngol Otol 116: 170-175.
- Moriariu I, Dias A, Curran A (2012) Giant parotid pleomorphic adenoma in the parapharyngeal space causing severe obstructive sleep apnoea. Ir Med J 105: 184-185.
- Mulla O, Agada F, Dawson D, Sood S (2013) Deep lob parotid pleomorphic adenoma presenting as obstructive sleep apnoea. BMJ Case Rep 2013: bcr2013008655.
- Mulla O, Agada F, Dawson D, Sood S (2011) Obstructive sleep apnoea and snoring-is examination necessary? Aust Fam Physician 40: 886-888.
- Adams AJ, Patterson AR, Brady G, Whitfield PH (2008) Resolution of obstructive sleep apnoea after resection of a pleomorphic salivary adenoma. Br J Oral Maxillofac Surg 46: 53-54.
- Yilmaz AD, Uniu E, Orbay H, Sensoz O (2006) Giant pleomorphic adenoma of soft palate leading to obstruction of the nasopharyngeal pot. J Craniofac Surg 17: 1001-1004.
- Giddings CEB, Bray D, Rimmer J, Williamson P (2005) Pleomorphic adenoma and severe obstructive sleep apnoea. J Laryngol Otol 119: 226-229.
- Motomura H, Harada T, Muraoka M, Taniguchi T (2000) Elongated uvula with a pleomorphic adenoma: a rare cause of obstructive sleep apnea syndrome. Ann Plast Surg 45: 61-63.
- Murthy SV, Murthy NC, Belagavi CS, Munishwara GB (2003) A large pleomorphic adenoma of soft palate causing sleep apnea syndrome-a case report. Indian J Pathol Microbiol 46: 466-467.
- Payne RJ, Hier MP, Kost KM, Black MJ, Zeitouni AG, et al. (2005) High prevalence of obstructive sleep apnea among patients with head and neck cancer. J Otolaryngol 34: 304-311.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences