Eyes See What Mind Knows: Fibrodysplasia Ossificans Progressiva, a Mimicker of Spondyloarthritis
Roshila Shamim1*, Asadullah Khan2, Saira Elaine Anwer Khan3, Muhammad Zeeshan Aslam4, and Arfa Talia55,
1Department of Rheumatology, Imam Clinic, Karachi, Pakistan
2Department of Rheumatology, Bollan Medical College, Civil Hospital, Quetta, Pakistan
3Department of Rheumatology, Shalamar Institute of Health Sciences, Lahore, Pakistan
4Department of Medicine, Punjab Medical College, DHQ Civil Hospital, Faisalabad, Pakistan
5Department of radiology, Fatima Memorial Hospital, College of Medicine and Dentistry, Lahore, Pakistan
*Corresponding Author:
- Roshila Shamim, Department of Rheumatology, Fatima Memorial Hospital, Imam Clinic, Karachi, Pakistan Email: rosh.shm@gmail.com
Received date: May 24, 2022, Manuscript No. IPRDDT-22-12517; Editor assigned date: May 26, 2022, PreQC No. IPRDDT-22-12517 (PQ); Reviewed date: June 09, 2022, QC No. IPRDDT-22-12517; Revised date: June 17, 2022, Manuscript No. IPRDDT-22-12517 (R); Published date: June 24, 2022 , DOI: 10.36648/2380-7245.8.6.45
Citation: Shamim R, Khan A, Khan SEA, Aslam MZ and Talia A (2022) Eyes See What Mind Knows: Fibrodysplasia Ossificans Progressiva, a Mimicker of Spondyloarthritis. J Rare Disord Diagn Ther Vol.8 No.6: 45.
Abstract
Introduction
Fibrodysplasia ossificans progressiva is a rare congenital disorder characterized by progressive heterotopic ossification of the connective tissue structures. The axial skeleton involvement and progressive limitation makes it a close mimicker of axial spondyloarthritis.
Case report
We report a case of 46-year old woman with a history of progressive limitation of different body regions starting as scoliosis of the chest, spreading to neck limitation, and then progressively involving the limitation of different regions in a proximal to distal pattern with sparing of distal limbs. Radiographic evaluation revealed calcification of different muscles, and ligaments in both axial and peripheral skeleton, with normal metabolic bone panels, and normal sacroiliac joints.
Conclusion
Fibrodysplasia ossificans progrressiva is a close mimicker of Axial Spondyloarthritis in terms of clinical and some of the radiological features, encountered in clinical practice.
Introduction
Fibrodysplasia Ossificans Progressiva (FOP) also called Myositis Ossificans Progressiva (MOP) is a rare genetic disorder of debilitating skeletal malformation. The disease has autosomal dominant inheritance with variable prominence in sporadic cases. A mutation in Activin Receptor IA/Activin-Like Kinase 2 (ACVR1/ALK2), a bone morphogenetic protein type I receptor, is believed to be the causative insult of FOP [1]. Pathophysiology of FOP involves a phenomenon of new bone formation [2]. The disease clinically manifests as episodes (flares) of inflammation of a specific region of the body initially manifesting as edema, followed by ossification and limitations of that region [3]. Trauma may be the trigger of flares. Although no treatment is of proven benefit, anti-inflammatory treatment, like steroids, bisphosphonates and ascorbic acid have all been tried with variable results. Striking involvement of Axial skeleton initially makes it a close mimicker of Axial Spondyloarthritides (SpA), which preferentially involve axial spine manifesting as spondylosis or fusion of spine.
We present here a case of FOP, the aim of reporting this case was to elaborate the close clinical mimicry of FOP with long standing axial spondyloarthritis.
Case Report
Our patient was a 46-year-old married lady, attended at the Department of Rheumatology, Fatima memorial hospital Shadman, Lahore, Pakistan. She had presented to us with complaints of progressive episodic hardening and limitation of different body parts, starting from her jaw, progressing to neck, elbows, hips and knees over a span of 30 years. Beside her chest bending to right side (scoliosis), she was alright till age 16 years. She developed swelling of neck and lock jaw at age 16 with associated symptoms of neck pain. Her symptoms of pain resolved, but left a residual decreased mouth opening of one finger only. Remaining asymptomatic in between, she developed progressive attacks of swelling and hardening of different body regions, starting from bilateral shoulders, then elbows, both hip and lately both knee joints. Her wrists and feet were not involved yet. All her attacks used to resolve after 4-6 weeks of pain and swelling, leaving behind the limitation of the involved area. Past history was significant for progressive bending forward of her spine.
Examination showed a lady of thin built, with shiny skin, over her arms, face, shoulders, neck and knees. She had decreased mouth opening, with no jaw movements. There was no movement in her neck in any plane. Both shoulders were fixed in flexed adducted position. Both elbows were fused at 90° in mid prone position. Her Hip joints were in slightly flexed position with no movements. Knees were in a slight flexed position with minimal movements in the coronal plane. Wrists, ankles, and small joints of the extremities were fully functional and had no limitation. On palpation, there were hard nodular masses palpable in both thighs anteriorly and lateral. Chest movements were severely restricted and respiratory movement was only diaphragmatic. Rest of her clinical examination was unremarkable.
Most of laboratory tests including panel for metabolic bone diseases were normal; Hemoglobin 11g/dl, TLC 8000/ml, Platelets 280 thousand/ml, serum creatinine 0.6mg/dl, Alanine Transaminase 34U/L, Alkaline Phosphatase 180U/L, Serum Calcium, 8.8mg/dl (corrected for Albumin), Phosphate 3 mg/dl, serum Parathyroid 43pg/ml, Vitamin D level 21ng/ml. Both ESR and C Reactive Protein (CRP) were within normal range. Her ANA profile and ENA profiles were negative.
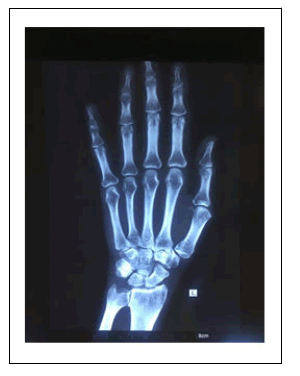
X rays showed diffuse generalized osteopenia of bones, along with calcification of myofascial tissues of different body regions in following pattern; periarticular calcification with complete joint ankylosis of Temporomandibular joint, scoliosis and fusion of lumbar spine, joint changes other than ankylosis in bilateral shoulder, elbow, Hip and knee joints, calcification of paraspinal, thigh and calf muscles [Figure 1]. However, her wrist, ankle and small joints of all four extremities were normal with no articular or periarticular changes [Figure 2]. Of special concern were sacroiliac joints which showed normal joint space, with no features of sacroiliitis [Figure 3].
The patient was counselled about the nature of disease and treated with short course of steroids and bisphosphonates. Detailed counselling of diet and ambulation was done by a nutritionist and physiotherapist respectively. Special emphasis on avoidance of trauma (both accidental and iatrogenic) was advised.
Discussion
FOP is a rare genetic disease clinically manifesting as myofascial calcification due to heterotopic ossification [2]. We present a case of FOP which as per literature search is first ever case reported by Rheumatology department to the best of our knowledge.
Our reported case is of peculiar clinical interest for a number of reasons. First, we want to emphasize the clinical mimicry of our case with axial Spondyloarthropathies (SpA). Progressive limitation of axial spine with peripheral joint involvement is a characteristic feature of both Ankylosing spondylitis and other spondyloarthritis [4]. Other mimickers include Diffuse Idiopathic Hyperostosis (DIH), calcification related to malignant hyperparathyroidism, osteitis condensans ilii are reported more commonly than FOP likely due to their comparatively common prevalence [5]. Unlike other mimickers, the disease in FOP is more extensive and not confined to pelvis (Osteitis condensans ilii), or spine alone (DIH) [6,7]. The radiographs of axial spine are usually confusing in cases of FOP; however, normal or nearly normal Sacroiliac joints make SpA a less likely possibility.
Second, the clinical manifestations of our case are characteristically unique. To start with, majority of the reported cases occur at an early pediatric age of less than 10 years, with a major percentage occurring in infancy and there is characteristic congenital malformation of big toes. Our patient had experienced her first complaint of pain and swelling of neck at the age of 16 years, which is rarely reported and lacks the classical pathognomonic sign of absent or dysmorphic first toe [Figure 4]. In addition, majority of the patients reported in literature had bony projections in subcutaneous tissues [8] our case lacks such bony projections both as symptoms and clinical findings. The likely cause could be her calcification along the axial planes initially, not noticed as a separate symptom.
To conclude, FOP is a close mimicker of axial spondyloarthritis, and should be considered when evaluating patients with long term spinal fusion, to prevent such patients from getting long term ineffective treatment.
Refernces
- Shore EM, Xu M, Feldman GJ, Fenstermacher DA, Cho TJ, et al. (2006) A recurrent mutation in the BMP type I receptor ACVR1 causes inherited and sporadic fibrodysplasia ossificans progressiva. Nat Genet 38: 525-527.
[Crossref], [Google Scholar], [Indexed] - Kitterman JA, Kantanie S, Rocke DM, Kaplan FS (2005) Latrogenic harm caused by diagnostic errors in fibrodysplasia ossificans progressiva. Pediatrics 116: 654-661.
[Crossref], [Google Scholar], [Indexed] - Pignolo RJ, Kaplan FS (2018) Clinical staging of Fibrodysplasia Ossificans Progressiva (FOP). Bone 109: 111-114.
[Crossref], [Google Scholar], [Indexed] - Sundstrom B, Ljung L, Hornberg K, Wallberg Jonsson S (2020) Long-term spinal mobility in ankylosing spondylitis: A repeated cross-sectional study. Arthritis Care Res 72: 1022-1028.
[Crossref], [Google Scholar] - Slobodin G, Lidar M, Eshed I (2017) Clinical and imaging mimickers of axial spondyloarthritis. Semin Arthritis Rheum 47: 361-368.
[Crossref], [Google Scholar], [Indexed] - Olivieri I, Gemignani G, Camerini E, Semeria R, Christou C, et al. (1990) Differential diagnosis between osteitis condensans ilii and sacroiliitis. J Rheumatol 17: 1504-1512.[Crossref],[Google Scholar], [Indexed]
- Taljanovic MS, Hunter TB, Wisneski RJ, Seeger JF, Friend CJ, et al. (2009) Imaging characteristics of diffuse idiopathic skeletal hyperostosis with an emphasis on acute spinal fractures. AJR Am J Roentgenol 193: 10-19.
[Crossref], [Google Scholar], [Indexed] - Kamal AF, Novriansyah R, Rahyussalim, Prabowo Y, Siregar NC (2015) Fibrodysplasia ossificans progressiva: Difficulty in diagnosis and management a case report and literature review. J Orthop Case Rep 5: 26–30.
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences