Paraneoplastic Pancytopenia Revealing Non-small Cell Lung Carcinoma
Moubachir H, El Khettabi W , Arfaoui H , Qachouh A , Diop Lacombe S , Jabri H and Afif MH
DOI10.21767/2380-7245.100050
1Department of Respiratory Diseases, Faculty of Medicine, Ibn Zohr University, Agadir, Morocco
2Department of Respiratory Diseases, Faculty of Medicine, Hassan II University, Casablanca, Morocco
3Department of Clinical Hematology, Faculty of Medicine, Hassan II University, Casablanca, Morocco
- *Corresponding Author:
- Houda Moubachir
Department of Respiratory Diseases, Faculty of Medicine
Ibn Zohr University, Agadir, Morocco
Tel: +212634600735
E-mail: moubachirhouda@gmail.com
Received date: September 05, 2016; Accepted date: October 03, 2016; Published date: October 10, 2016
Citation: Moubachir H, Khettabi WEl, Arfaoui H, et al. Paraneoplastic Pancytopenia Revealing Non-small Cell Lung Carcinoma. J Rare Disord Diagn Ther. 2016, 2:5. doi:10.21767/2380-7245.100050
Copyright: © 2016 Moubachir H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
syndromes (PNS) are defined as clinical syndromes implying non-metastatic systemic effects accompanied malignant tumor. pancytopenia is rare. Some manifestation of hematological PNS associated to hematological system cells and cogulation factors are coagulopathy, anemia, granulocytosis, granulocytopenia, thrombocytosis and thrombocytopenia. This observation presents a case of pancytopenia revealing non-small cell lung carcinoma.
Keywords
Lung carcinoma; Lung consolidation; Paraneoplastic syndromes; Pancytopenia
Observation
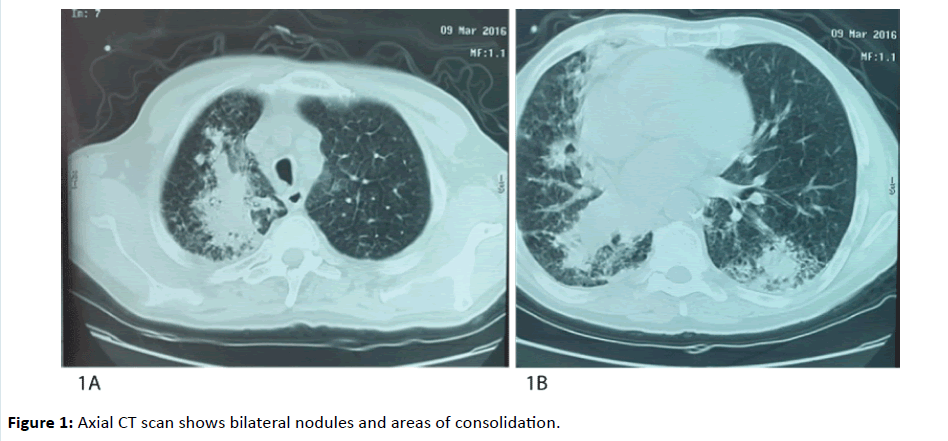
A 56 year old patient, chronic smoker and cannabis user with withdrawn four years ago, without any particular pathological antecedent, complains since two months of dyspnea worsening progressively even to small effort, a cough associated with low abundance hemoptysis, in a context of asthenia, fever and weight loss. On examination, the patient’s performance status (PS) was at three, fever at 100.4 Fahrenheit (°F), tachycardia at 100 beats per minute, polypnea at 28 cycles per minute, desaturated at 80%, an important conjunctival palor, and no petechial or cutaneous eruption. Complete blood count (CBC) done in emergency objectivated pancytopenia with anemia (hemoglobin at 84 g per deciliter (g/dL)) normochromic, normocytic, white blood cells at 1.100 per microliter of blood (μL), with neutrophils at 400/μL, lymphocytes at 610/μL, and platelets at 51.000/μL. Chest CT scan objectivated bilateral consolidation associated to bilateral mediastinal and hilar adénopathies (Figures 1A and 1B).
The C-reactive protein was at 268 mg/L, lactico-deshydrogenase (LDH) was normal at 204 units per liter (UI/L). The infectious balance was negative. The patient received oxygen therapy, large spectrum antibiotics, and transfusion. Bronchoscopic exploration objectivated an inflammatory status at the entrance of the right lobar bronchus, associated to an endobronchial tumor bud, completely obstructing the middle lobar bronchus, which is incatheterisable. The anatomopathologic and immunohistochemistry studies of bud biopsies concluded to a primitive undifferentiated adenocarcinoma of lung. The carcimoma classified stage four of the tumor, node, and metastasis (TNM) classification of lung cancer. The serology of Human Immunodeficiency Virus.
(HIV), hepatitis B and C were negative. The myelogram has objectivated a poor bone marrow with some myeloid cells and some plasmocytes concluding to medullary aplasia. The palliative chemotherapy couldn’t be started because of the impaired condition of the patient and the advanced stage of the disease. The patient died in respiratory distress a few days after diagnosis.
Discussion
This observation illustrated medullary aplasia associated with bronchogenic cancer. This association has multiple possible explanations: Both diseases are not related to each other, or pancytopenia is secondary to lung carcinoma, in a context of hematological paraneoplastic syndrome or metastatic. Pancytopenia in patients with malignant tumors without evidence of bone marrow metastasis is extremely rare, and in those patients, the bone marrow is generally hypocellular. Paraneoplastic syndrome is a term used for the tumor’s indirect system effects [1-4]; it has diagnosis and therapeutic problem [5].
The most known hematologic paraneoplastic syndromes are: anemia, leukocytosis with leukemoid reaction, polyglobulia, thrombocyts, and hypercoagulability [3-7]. This can only be proven without any doubt if the pancytopenia has improved after curative treatment of the tumor. Unfortunately, because of the metastatic stage and the impaired condition of the patient at diagnosis time, the patient was unable to tolerate chemotherapy, and the paraneoplastic character couldn’t be confirmed. There is no decisive test for paraneoplastic syndromes identification; it’s diagnosis of exclusion. An important characteristic of PNS associated with tumor is the influence of curative therapy on symptoms. Partial or complete responses to chemotherapy or radiotherapy can be seen [8]. Unfortunately, the aggressive character of bronchogenic carcinoma and the advanced stages at diagnosis time make curative treatment rarely indicated, and we rarely see a regression of PNS. Raz et al. [9] have reported three followed cases for pancytopenia that have developed lung cancer in the two year of follow up period. One of the cases had partially showed an improvement of pancytopenia at the beginning of chemotherapy, but unfortunately, passed away during therapy. The two other cases died before starting treatment.
Conclusion
The PNS creates a diagnosis issue with metastasis. It has to be taken in consideration in differential diagnosis. Even though pancytopenia is a rare hematological PNS, it has to be explored because of possible malignancy associated for an early management.
References
- Cosar-Alasa R, Yurut-Caloglua V, Karagolb H, Caloglua M, Yalcin O, et al. (2007) Paraneoplastic syndrome of non-small cell lung carcinoma: A case with pancytopenia, leukocytoclastic vasculitis, and hypertrophic osteoarthropathy. Lung Cancer 56: 455-458.
- Arnold MS, Patchell R (2001) Paraneoplastic syndromes. Cancer principles and practice of oncology (6th edn.) Lippincott Williams & Wilkins, Philadelphia pp: 2511-2536.
- Helbig W (1970) Importance of paraneoplastic bone marrow and blood picture findings. Verh Dtsch Ger Inn Med 86: 428-432.
- Thomas C (1975) Das paraneoplastische syndrome. Med Klin 70: 2053-2065.
- Gerber RB, Mazzone P, Arroliga AC (2002) Paraneoplastic syndromes associated with bronchogenic carcinoma. Clin Chest Med 23: 257-264.
- Payan HM, Gilbert EF, Mattson M (1978) Hematological and biochemical paraneoplastic disorders. Arch Pathol Lab Med 102: 19-21.
- Hammond D, Winnick S (1974) Paraneoplastic erythrocytosis and ectopic erythropoietins. Ann NY Acad Sci 230: 229-228.
- Suzuki M, Kimura H, Tachibana I, Fujimura H, Nakatsuji Y, et al. (2001) Improvement of anti-Hu-associated paraneoplastic sensory neuropathy after chemoradiotherapy in a small cell lung cancer patient. Intern Med 40: 1140-1143.
- Raz I, Shinar E, Polliack A (1984) Pancytopenia with hypercellular bone marrow a possible paraneoplastic syndrome in carcinoma of the lung: a report of three cases. Am J Hemtol 16: 403-408.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences