Acanthamoeba Keratitis: Diagnosis and Treatment
Shriram H Bairagi
DOI10.21767/2380-7245.100061
Shriram H Bairagi*
Department of Pharmaceutical Chemistry, Ideal College of Pharmacy and Research, Mumbai, India
- *Corresponding Author:
- Bairagi SH
Assistant Professor
Department of Pharmaceutical Chemistry
Ideal College of Pharmacy and Research
Mumbai, 421306, India
Tel: +917715031328
E-mail: shrirambairagi@gmail.com
Received Date: July 13, 2017; Accepted Date: July 14, 2017; Published Date: July 19, 2017
Citation: Bairagi SH (2017) Acanthamoeba Keratitis: Diagnosis and Treatment. J Rare Disord Diagn Ther. 3:8. doi: 10.21767/2380-7245.100061
Introduction
Acanthamoeba species are the causative agent of a sight threatening infection of the cornea known as Acanthamoeba keratitis, caused by the free-living amoeba Acanthamoeba spp., and is a sight-threatening corneal infection that presents with corneal ulcerations. It was first reported in 1973 [1]. Acanthamoeba are ubiquitous protozoa that exist in 2 forms: Trophozoites (the active form) and cysts (the inactive form). Cysts are notoriously difficult to kill and this is one reason why this infection is so difficult to eradicate. Only one class of medications is known to have cystocidal activity, the biguanides. The incidence of Acanthamoeba keratitis in this study was found to be 1.04% and the incidence in other reported Indian series ranges from 0.34 to 1.4% [2-5].
The incidence of Acanthamoeba keratitis appears to be increasing because of its frequent association with contact lens wear, which represents the cause of >85% of Acanthamoeba keratitis cases, especially in developed countries [6-8]. Members of the genus Acanthamoeba are ubiquitous and can be isolated from well, tap, bottled and swimming pool water, as well as sand, dust, human nasal and throat secretions, and animal stools. The life cycle of Acanthamoeba consists of a trophozoite and a cyst stage [9].
Diagnosis and Detection
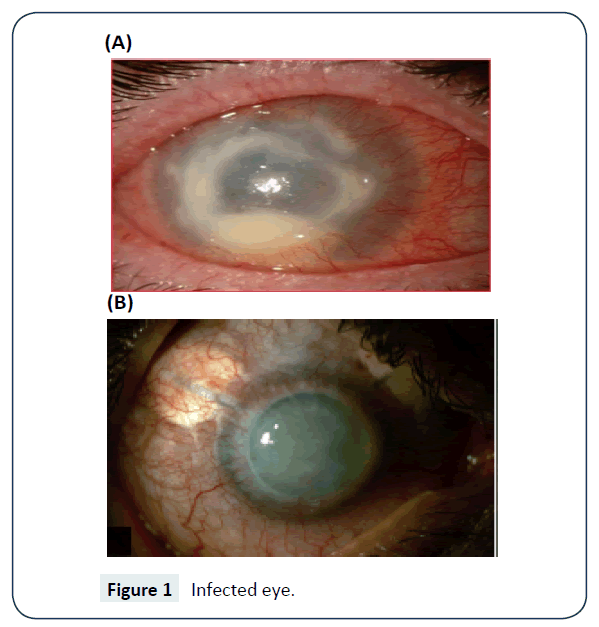
The detection can be done in laboratory using non nutrient agar saline plate seeded with gram negative bacteria such as Escherichia coli. The PCR is used to confirm the diagnosis especially when the contact lenses are involved. Molecular methods also available for detection and identification of Acanthamoeba, these methods are also suitable for both clinical and epidemiological purposes [10,11]. The fluorescent in situ hybridization technique has also been successfully employed for the purpose detection [12]. Figure 1 shows the infected eye.
Treatment and Case Studies
Acanthamoeba is difficult to treat, but effective management can save ones eye. Topical anti-infective agents used in early-stage, surgical intervention is necessary in later stages. Propamidine 0.1% and neomycin 1% shows good activity against AK Since then, two or more topical anti-amoebic agents are used throughout the day. Polyhexamethylene Biguanide (PHMB, 0.02%) and chlorhexidine (0.02%), are effective in both monotherapy and combination therapy with a diamidine [13].
Case studies show that the Acanthamoeba keratitis is successfully treated in the person having the contact lens using six month therapy with topical Miconazole, Metronidazole, Prednisolone and neomycin as well as oral ketokonazole. In another case of person without contact lens having burning sensation the additional use of Propamidine in the above therapy shows the improvement in the corneal ulcer. In another case where topical Tobramycin and Cefazolin added in the therapy [14]. The combination of Dibromopropamidine and Propamidine isethionate ointment and drops and neomycin drops are used successfully in the 44 years old patient having corneal infection from Acanthamoeba species [15].
Bilateral Acanthamoeba keratitis was successfully treated with Chlorhexidine, Polyhexamethylene biguanide, Propamidine ise-thionate in combination with Atropine and Dibromopropamidine an improvement was noted at which point Atropine and Dibromopropamidine were stopped while Fluorometholone acetate, Acyclovir and Ciprofloxacin were prescribed and patient was discharged [16]. Few studies state that addition of the neomycinpolymyxin B also gives the good result [17].
Prevention
Mostly the Contact lens wearers need to take precaution while cleaning the lenses should never use the tap water and saline to clean. As the treatment is toxic and lengthy so they should visit if they find out some sign of inflammation. And those without lenses they should not wash their eyes with lake or sea water.
References
- Illingworth CD, Cook SD (1998) Acanthamoeba keratitis. Surv Ophthalmol 42: 493-508.
- Manikandan P, Bhaskar M, Revathy R, John RK, Narendran V, et al. (2004) Acanthamoeba keratitis: A six year epidemiological review from a tertiary care eye hospital in South India. Indian J Med Microbiol 22: 226-230.
- Srinivasan M, Gonzales CA, George C, Cevallos V, Mascarenhans JM, et al . (1997) Epidemiology and etiological diagnosis of corneal ulceration in Madurai, South India. Br J Ophthalmol 81: 965-971.
- Leck AK, Thomas PA, Hagan M, Kalimurthy J, Ackuaku E, et al . Aetiology of suppurative corneal ulcers in Ghana and South India and epidemiology of fungal keratitis. Br J Ophthalmol86: 1211-1215.
- Basak SK, Basak S, Mohanta A, Bhowmick A (2005) Epidemiological and microbiological diagnosis of suppurative keratitis in Gangetic West Bengal, Eastern India. Indian J Ophthalmol 53: 17-22.
- Patel A, Hammersmith K (2008) Contact lens-related microbial keratitis: recent outbreaks. Curr Opin Ophthalmol 19: 302-306.
- Thebpatiphat N, Hammersmith KM, Rocha FN (2007) Acanthamoeba keratitis: a parasite on the rise. Cornea 26: 701-706.
- Verani JR, Lorick SA, Yoder JS (2009) National outbreak of Acanthamoeba keratitis associated with use of a contact lens solution, United States. Emerg Infect Dis 15: 1236-1242.
- DE Jonckheere (1991) JF: Ecology of Acanthamoeba. Rev Infect Dis 13: S385-S387.
- Pasricha G, Sharma S, Garg P, Aggarwal R (2003) Use of 18S rRNA Gene-Based PCR Assay for Diagnosis of Acanthamoeba Keratitis in Non-Contact Lens Wearers in India journal of Clinical Microbiology 41: 3206-3211.
- Schroeder JM, Booton GC, Hay J, Niszl IA, Seal DV, et al. (2001) Use of subgenic 18S ribosomal DNA PCR and sequencing for genus and genotype identification of acanthamoebae from humans with keratitis and from sewage sludge. J Clin Microbiol 39: 1903-1911.
- Stothard DR, Hay J, Schroeder-Diedrich JM, Seal DV, Byers TJ (1999) Fluorescent oligonucleotide probes for clinical and environmental detection of Acanthamoeba and the T4 18S rRNA gene sequence type. J Clin Microbiol 37: 2687-2693.
- Wright P, Warhurst D, Jones BR (1985) Acanthamoeba keratitis successfully treated medically. Br J Ophthalmol 69: 778-782.
- Duff D, Horne MD, Mary EF (1994) Acanthamoeba keratitis: an emerging clinical Problem. Can Med Assoc J 150: 1.
- Wright P, Warhurst D, Barrie R (1985) Acanthamoeba keratitis successfully treated medically. Br J Ophthalmol 69: 778-782.
- Hassanlou M, Bhargava A, Hodge WG (2006) Acanthamoeba keratitis and treatment strategy based on lesion depth. Can J Ophthalmol 41: 71-73.
- Wang IJ, Hong JP, Hu FR (1997) Clinical features and outcome of Acanthamoeba keratitis. J Formosan Med Assn 96: 895-900.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences